Laparoscopic surgery provides relief for teenage patient with adenomyoma and endometriosis
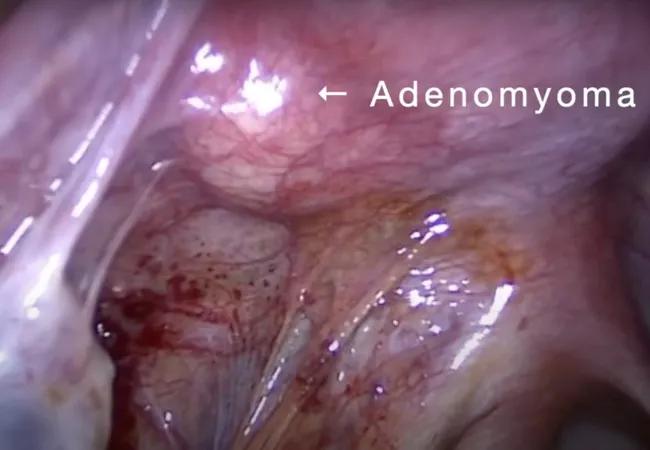
When medical therapy provided minimal relief for a 16-year-old with chronic pelvic pain and dysmenorrhea, the patient’s gynecologist referred her to experts in Cleveland Clinic’s Ob/Gyn & Women’s Health Institute. After a multidisciplinary team discovered the patient had a juvenile cystic adenomyoma and concomitant endometriosis, she elected to undergo laparoscopic surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This case is interesting because of the patient’s age and the pathology,” says Angelina Carey-Love, MD, a physician in the Department of Obstetrics and Gynecology. “Focal adenomyosis is fairly uncommon, especially in combination with endometriosis. Medical management is an option, but it doesn’t always work. Surgery is indicated in certain circumstances.”
Dr. Carey-Love and three colleagues published a video presentation of surgical techniques for excision of juvenile cystic adenomyoma in the American Journal of Obstetrics & Gynecology, as well as on YouTube.
The patient’s gynecologist prescribed birth control pills, a common first line of therapy, when the young woman originally complained of pain accompanying her periods.
“A lot of patients have primary dysmenorrhea, but there can be secondary causes, including adenomyosis, endometriosis, congenital anomalies, cysts and pelvic inflammatory disease,” says Dr. Carey-Love.
The pain persisted for 18 months, so the gynecologist ordered an ultrasound, which revealed a 2.4 cm lesion in the left adnexa. The gynecologist performed a diagnostic laparoscopy, but couldn’t discern the lesion internally. So the patient was referred to reproductive, endocrinology and infertility (REI) specialists at Cleveland Clinic.
The REI physicians started the patient on leuprolide acetate, a gonadotropin-releasing hormone (GnRH) medicine. However, the pain continued and subsequent imaging studies revealed a T2-hypointense round lesion in the posterior myometrium, now smaller, measuring 1.1 cm.
Advertisement
“Since the patient was still in pain, she was offered and desired surgical management,” says Dr. Carey-Love, who is part of the Minimally Invasive Gynecologic Surgery (MIGS) team. The patient was taken off of leuprolide acetate, which had the side effect of shrinking the lesion, so it would grow and be easier to locate during surgery.
Three months later, teams from MIGS and REI collaborated on the 2 ½-hour, minimally invasive surgery. They performed a hysteroscopy to fully examine the cervix and uterus, then laparoscopically resected the adenomyoma and excised pelvic endometriosis lesions. The patient was placed on hormonal suppression post-operatively, and she is doing well, with only minor cramping during her menses. “A multidisciplinary approach was essential to successful diagnosis and treatment,” says Dr. Carey-Love. “Healthcare providers from REI, MIGS and medical imaging all worked together.”
Dr. Carey-Love shared surgical techniques for excision of adenomyomas in her video presentation to create awareness about the condition and encourage other physicians in MIGS to consider the procedure when appropriate.
“Surgeons don’t need to be at a large tertiary center. Anyone who is confident in their laparoscopic skills and pelvic anatomy can perform this procedure,” she says. “If they follow the critical steps, then they can successfully treat patients.”
Dr. Carey-Love highlights four key points about the technique:
Advertisement
She also shares a message with gynecology peers about pain. “Unfortunately, pain with menses is normalized, and many patients get into their 30s and 40s living unnecessarily with pain,” says Dr. Carey-Love. “If you are treating a patient with persistent pain, don’t be afraid to bring other physicians on board to figure it out. We need to change the way we think about pain.”
Advertisement
Advertisement

Benefits include reduced pain, earlier mobilization and more likely discharge to home

Addressing the brain-body interplay can help patients achieve better outcomes

Alzheimer’s studies delve into sex-related variances in the expression of the disease

Approximately 500 million people globally are experiencing 'period poverty'

Pediatric and adolescent reproductive providers are uniquely positioned to intervene

Personalized reconstruction is an alternative to leg amputation or flail limb

Women’s Comprehensive Health and Research Center addresses unmet needs

A Q&A with Cara King, DO, MS, on the upleveling power of coaching