Surgical video highlights techniques for optimizing myomectomy
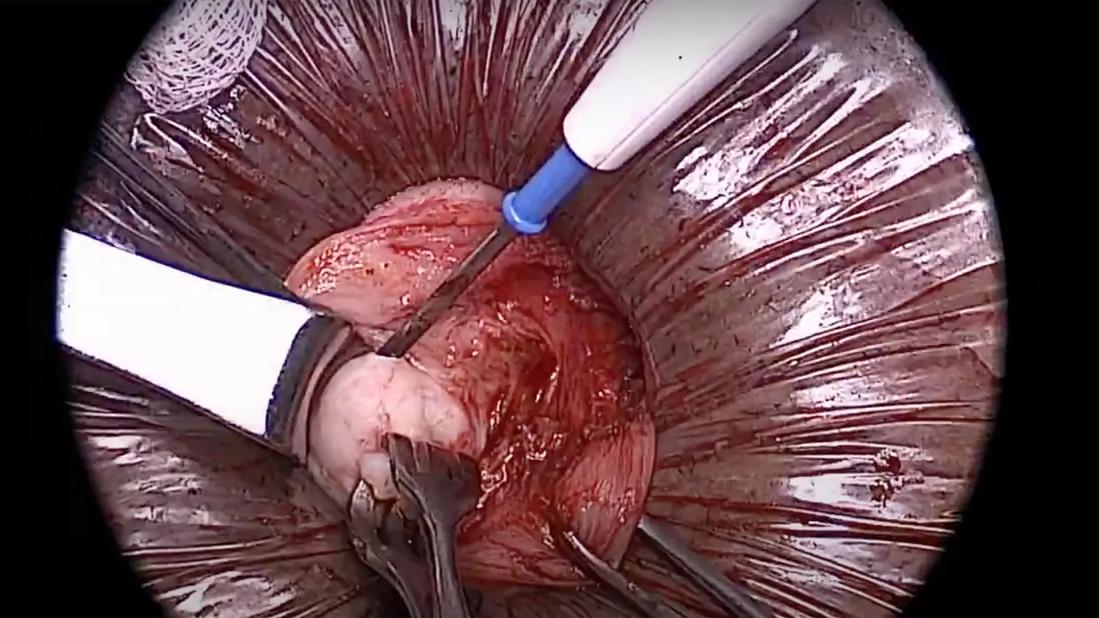
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d0cb5d7d-0a4e-4491-a3da-2435b409f873/minilaparotomy-myomectomy)
image from mini-laparotomy
When the abundance or location of a patient’s uterine fibroids make laparoscopic surgery difficult, the mini-laparotomy can be a better minimally invasive fertility-sparing option. Yet some surgeons may overlook the mini-lap in favor of a more invasive procedure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To highlight the potential of the technique, specialists at Cleveland Clinic’s Obstetrics & Gynecology Institute created a brief demonstration video using intraoperative images.
“Typically for people who desire future pregnancy, we do laparoscopic myomectomy all the time, which means through 5-millimeter incisions,” says Cara King, DO, who published the video with colleagues. “But for some patients, with increased fibroid number or large size, a laparoscopic approach is difficult. That’s when a mini-laparotomy may be appropriate.”
Although there’s no strict incision metric that defines a mini-laparotomy, Dr. King says she and her colleagues consider it to be about 4 centimeters or smaller. Anything much bigger is considered a laparotomy.
“The goal of the video is to show how much can be done through an incision that's only 3 to 4 centimeters,” she says. “For these big myomectomies, you don't have to make a big incision. In many cases, patients are going home the same day; there’s no hospital admission. We just want to help other surgeons feel comfortable in starting to incorporate this approach into their practice.”
The video highlights 10 techniques. Among them:
Direct palpation of fibroids
Although Cleveland Clinic surgeons use MRI mages to map fibroid locations before surgery, smaller ones can be difficult to see. “Feeling with our hands can be really helpful,” says Dr. King. “With laparoscopy, you get some tactile sense through your instruments. Robotic surgery offers less tactile feedback. Mini-laparotomy allows you to use your hands to feel where the endometrial cavity is and if there are extra fibroids behind where you just took one out. It can be beneficial in making sure you don't miss any.”
Advertisement
Use of a uterine manipulator to visualize the endometrial cavity
“We use uterine manipulators and inject blue dye into the uterine cavity,” says Dr. King. “If the cavity is intact, the dye stays in. If that cavity has a defect from the myomectomy, they dye comes out through that defect. That provides immediate feedback, so we can address it. How big is that defect? What’s the best way to repair it? You’re typically doing this procedure to preserve future fertility, so you want to make sure this uterus is ready for pregnancy.”
Suture technique that avoids the endometrial cavity
Some surgeons are dissuaded from doing a minimally invasive technique for myomectomy because of the amount of suturing required. “If you can't suture efficiently robotically, or you can't suture efficiently laparoscopically because you're avoiding the endometrial layer, a mini-laparotomy can be a good technique,” says Dr. King. “It's a good in-between for people who may not have the skillset to be doing things laparoscopically but want to avoid creating a big incision.”
In addition to providing guidance for peers, Dr. King says it’s important to be an advocate for patients.
“Sometimes a patient will see a surgeon who says they need to have their uterus out and not offer a myomectomy because they don’t have the skill set,” she says. “My message is always that when patients with fibroids want to retain fertility, they should seek a referral to a subspecialist. Sometimes the uterus can be saved. A subspecialist may be able to do that with a mini-laparotomy or a laparoscopic approach.”
Advertisement
Advertisement
ACOG-informed guidance considers mothers and babies
Psychological care can be a crucial component of medical treatment
A Q&A with Cara King, DO, MS, on the upleveling power of coaching
New guidelines let the patients steer the process
Specialized unit provides patients with faster, more targeted care
Clinical mentors and job rotations provide a view of opportunities
Nurses and doulas work together to care for expectant moms
Disease associated with higher risks for maternal and fetal morbidities