Study provides Class III evidence that assay distinguishes disease from normal controls
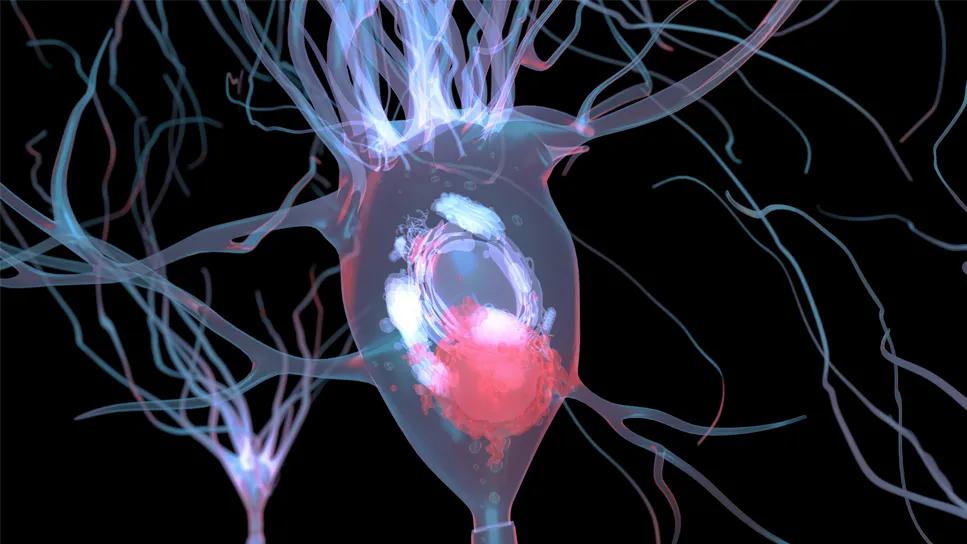
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/69fc9390-9c2f-4c21-a97e-1aa83bff4891/lewy-body-dementia-research-1034683308)
Lewy body in neuron affected by Parkinson’s disease
A positive result from the α-synuclein seed amplification assay (αSyn-SAA) — a qualitative test performed on cerebrospinal fluid (CSF) — is highly associated with clinical features of dementia with Lewy bodies (DLB), especially hyposmia (reduced sense of smell). So found a multicenter study comparing αSyn-SAA results between patients with clinically diagnosed DLB and neurologically healthy controls. The study was recently published in Neurology (2024;103[3]:e209656).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“DLB is particularly difficult to diagnose, and it is currently done primarily by clinical evaluation,” says Cleveland Clinic neurologist James Leverenz, MD, one of the study’s senior authors. “This study provides important evidence for improving diagnostic criteria as well as supporting the clinical use of a direct biomarker.”
Dr. Leverenz directs the Cleveland Clinic Lou Ruvo Center for Brain Health in Cleveland, which serves as coordinating site for the multicenter DLB Consortium. Part of the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program, the consortium facilitates collection of clinical data to support biomarker discovery to improve the diagnosis of DLB.
A DLB diagnosis can only be definitively confirmed at autopsy. Otherwise, diagnosis is based on core clinical features, including significant cognitive decline with fluctuations, parkinsonism, visual hallucinations and rapid eye movement (REM) sleep behavior disorder, with hyposmia being a supportive clinical feature. Currently used biomarkers to aid diagnosis — i.e., FP-CIT, MRI, cardiac MIBG and polysomnography — are indirect indicators of DLB.
Because some core symptoms may be subtle or absent, and because they overlap with symptoms of Parkinson’s disease, Alzheimer’s disease and other dementias, DLB is prone to under- and overdiagnosis.
The recently developed αSyn-SAA measures aggregates of a misfolded protein specific to Lewy bodies and Lewy neurites in the brain, making it a biomarker of interest for diagnosing DLB. Studies have indicated that αSyn assays are more than 90% sensitive and specific for autopsy-confirmed DLB and Parkinson’s disease, even in patients with a mixed clinical picture.
Advertisement
The newly published study was designed to determine whether αSyn-SAA can distinguish patients with clinically diagnosed DLB from normal controls, and to assess the association between αSyn-SAA positivity and clinical features used to diagnose DLB.
Three cohorts were created from patients in the DLB Consortium registry and other studies involved in the Parkinson’s Disease Biomarker Program from 2017 to 2021. They are:
All patients had CSF samples that had been drawn within 12 months of the baseline visit, and αSyn-SAA testing was performed for this study. Multiple samples over time were available for 82 participants; all but one had consistent αSyn-SAA results.
CSF αSyn-SAA was positive in 72% of the DLB cohort versus 4% of each control group. Of patients in the DLB cohort with at least two core clinical features of the disease (n = 156), 78% tested positive.
Results from multiple standardized clinical assessments were also analyzed. Among the DLB cohort, the following differences were observed between those who had a positive αSyn-SAA test compared with those who had negative results:
Advertisement
The most significant predictor of αSyn-SAA positivity was the UPSIT score: it was associated with the highest area under the curve (0.87; 95% CI, 0.81-0.94). Those who scored at or below the hyposmia threshold were 18.3 times more likely to have positive αSyn-SAA results (95% CI, 7.52-44.6) than age- and sex-matched patients with normosmia.
Results of this study provide Class III evidence that CSF αSyn-SAA distinguishes patients with clinically diagnosed DLB from normal controls, the authors concluded.
Dr. Leverenz notes that a significant fraction of patients with clinically diagnosed DLB did not have a positive αSyn-SAA result. Those who did test positive were more likely to have REM sleep disorder and worse hyposmia, cognitive impairment and parkinsonism. However, the presence of core features of visual hallucinations and cognitive fluctuations did not differ between those who did and did not test positive.
“We must consider that the current list of core features overdiagnoses DLB,” Dr. Leverenz says. “Based on our findings and other published reports, we recommend that clinical assessment place a higher value on hyposmia, which should be evaluated with an objective test such as the UPSIT.”
He adds that less invasive αSyn-SAA testing, via skin biopsies and blood samples, is currently being investigated.
Dr. Leverenz acknowledges the important contributions of the other sites, in addition to Cleveland Clinic, participating in the DLB Consortium, the NINDS Parkinson’s Disease Biomarkers Program and the Lewy Body Dementia Association: Barrow Neurological Institute, Columbia University, Rush University, Thomas Jefferson University, University of California San Diego, University of Miami, University of North Carolina, University of Pennsylvania, University of Pittsburgh, and VA Puget Sound Health Care System/University of Washington.
Advertisement
Advertisement
The disease’s neuropathologic heterogeneity holds clues to refining diagnosis and prognosis
Initiatives focus on the physical and emotional well-being of geriatric patients and their caregivers
Novel Cleveland Clinic project is fueled by a $1 million NIH grant
Large NIH-funded investigation is exploring this understudied phenomenon
Initial results show good accuracy of scalable, low-cost tool for flagging cognitive decline
Depression, agitation, delusions and more compound challenges for patients and caregivers
New tool for general neurologists aims to streamline differential diagnosis
Patient history plays a key role in identifying the condition