Proteins related to altered immune response are potential biomarkers of the rare AD variant
Rapidly progressive Alzheimer’s disease (rpAD) — which is associated with much faster cognitive decline and earlier mortality than the more common slower sporadic AD (spAD) phenotype — has distinct immune-related proteins in the brain and cerebrospinal fluid (CSF). The findings, recently published in Alzheimer’s Research & Therapy (2025;17[1]:118), raise the prospect of a biomarker test that could be developed to assist in diagnosis and clinical research of this AD variant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The proteins were identified after extensive proteomics research by investigators from the National Institute on Aging’s Cleveland Alzheimer’s Disease Research Center (CADRC), one of more than 30 such collaborative centers nationwide focused on AD.
“The heterogeneity of clinical manifestations of Alzheimer’s disease is reflected at a basic molecular level,” says the study’s senior and corresponding author, Jagan Pillai, MD, PhD, a neurologist in Cleveland Clinic’s Lou Ruvo Center for Brain Health and Director of CADRC, which has special expertise in the study of the rate of AD progression. “By identifying proteins that are found only in the rapidly progressive variant, we may be able to better understand underlying mechanisms and develop a diagnostic tool to distinguish this variant from the more common AD type as well as from other rapidly progressive dementias.”
The rpAD phenotype is characterized by rapid cognitive decline and survival duration of less than three years from diagnosis, compared with the typical 12 to 15 years with spAD. The rare rpAD variant has not been well studied, but distinct biological differences have been identified between the two phenotypes in APOE Ɛ4 allele frequency, tau seeding and amyloid plaque composition.
The CADRC study aimed to further characterize rpAD using proteomics, with the goal of identifying distinct protein signatures in the CSF to assist in development of a clinical biomarker test and to further elucidate underlying biological mechanisms.
Advertisement
“Our overall goal is to understand why the same neuropathology seen in rpAD and spAD — amyloid plaques and neurofibrillary tangles — can lead to such different outcomes,” Dr. Pillai explains. “We currently have no way to predict how rapidly disease will progress at the time of diagnosis.”
Eight patients with rpAD in this study (four female; mean age, 76 years) were identified from the National Prion Disease Pathology Surveillance Center. Although they had a rapid clinical course suggestive of Creutzfeldt-Jakob disease, they were found at autopsy to have no evidence of prion disease but instead had neuropathologic findings consistent with AD. All had died within three years of symptom onset.
In addition, three patients with spAD (two female; mean age, 76 years) were included for analysis. These patients were identified from the Case Western Reserve University Memory and Aging Center brain bank, with spAD defined as fulfillment of standard AD criteria, a predominance of amnestic symptoms and survival > 3 years from diagnosis.
Proteins co-aggregating with core-amyloid-β plaques were characterized from fresh frozen tissue taken from medial temporal regions in each of the 11 patients. Findings included the following:
Advertisement
Using Gene Ontology (GO) analysis, the study authors identified biological themes that distinguished rpAD from spAD proteins. Differences were found in DNA repair, telomere organization and epigenetic modifications — e.g., DNA methylation — that regulate gene expression, RNA activity and cellular processes.
“The next step is to try to validate the promising biomarker candidates we’ve identified in this research,” says Dr. Pillai. “We’ll be particularly interested to see if the presence of these proteins correlates with disease progression.”
The CADRC is following many patients longitudinally, and Dr. Pillai intends to use their data to inform this research.
He notes that it would also be useful to compare levels of the rpAD-specific proteins his group identified to established AD biomarkers such as phosphorylated tau, total tau and neurofilament light chain in the same cohort. Such research could reveal mechanisms of neurodegeneration in rpAD versus spAD, he explains.
“Results of the GO analysis were also intriguing in that they revealed pathways characteristic of rpAD that tend to be especially disruptive to brain health,” Dr. Pillai adds. “This suggests a variety of possible preclinical research investigations that could elucidate mechanisms of neuropathology and potentially lead to new therapeutics.”
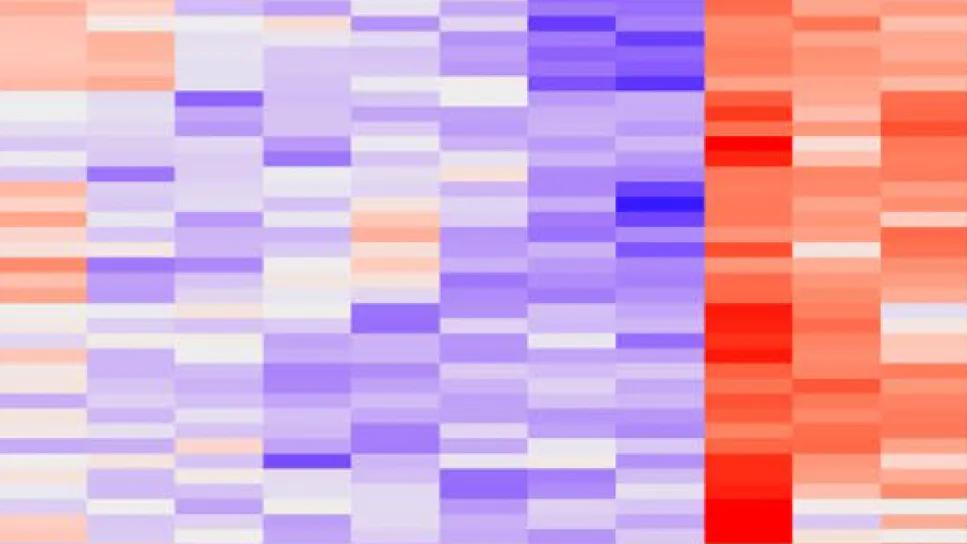
Image at top: Portion of a heatmap showing differentially expressed proteins and their association with Alzheimer's disease.
Advertisement
Advertisement

An expert talks through the benefits, limits and unresolved questions of an evolving technology

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

Large NIH-funded investigation is exploring this understudied phenomenon

Observational evidence of neuroprotection with GLP-1 receptor agonists and SGLT-2 inhibitors

Genomic study lays groundwork for insights into potential biomarkers and therapeutic strategies

Alzheimer’s studies delve into sex-related variances in the expression of the disease

Validated scale provides a method for understanding how lifestyle may protect against Alzheimer's

Collaborative approach may reduce distress caused by neuropsychiatric symptoms