Will enable sharper focus on new diagnostic tools for elusive neurodegenerative disease
The Dementia with Lewy Bodies Consortium is extending and expanding its collaborative research thanks to a new $10.7 million, five-year renewal grant to Cleveland Clinic from the National Institutes of Health (NIH). The national consortium, established in 2017 to improve the diagnosis and treatment of dementia with Lewy bodies, has centralized research efforts and created a coordinated registry for clinical data on the progressive neurodegenerative disorder.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Supported by the renewal grant, the consortium now includes collaborative sites Rush University, University of Pittsburgh, University of Pennsylvania, University of California San Diego (UCSD), University of North Carolina, the VA-Puget Sound Health Care System/University of Washington and Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas.
Led by principal investigator James Leverenz, MD, of Cleveland Clinic, the research team has added Oscar Lopez, MD, at University of Pittsburgh and Douglas Galasko, MD, at UCSD as co-principal investigators with a sharper focus on developing new tools to accurately diagnose dementia with Lewy bodies and related cognitive issues linked to Parkinson’s disease.
The consortium’s continuing research will build on its foundational work conducted under the initial five-year NIH grant that helped found the consortium. Its multicenter registry study aims to use longitudinal data from the expanded patient cohort to identify biomarkers that can assist with diagnosis, detection of disease progression and ultimately measurement of treatment response.
“Dementia with Lewy bodies is the second most common cause of dementia in the elderly, but it remains challenging to diagnose,” says Dr. Leverenz, Director of Cleveland Clinic’s Lou Ruvo Center for Brain Health in Cleveland. “Through our establishment of a national registry, we have generated a significant amount of data and biofluid samples that have been shared with investigators through a collaboration with the National Institute of Neurological Disorders and Stroke and the National Institute on Aging. With this new funding, we can now use that important information to improve diagnosis, identify biomarkers for disease and develop much-needed new therapies for patients.”
Advertisement
It has been estimated that more than 1.4 million people in the United States have dementia with Lewy bodies, yet no medications are approved to treat its symptoms and no current treatments offer meaningful hope for a cure.
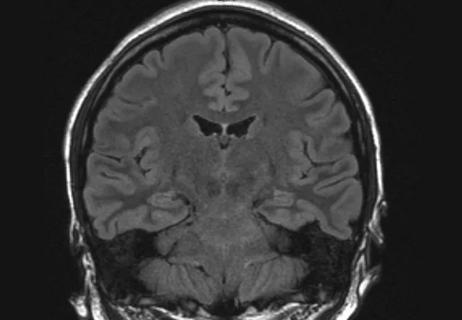
Through the consortium, researchers from the clinical sites have collected clinical information, imaging scans and biospecimens from more than 150 patients in a centralized database. The team analyzes the data to understand associations between patient characteristics and faster rates of decline over time to better predict outcomes.
“Research on dementia with Lewy bodies has previously been hindered by the need for large groups of patients to study in a consistent manner over time,” Dr. Leverenz notes. “Our consortium addresses this issue by bringing together a group of experts and providing the infrastructure to study a large number of patients from across the country. By expanding our collaborative research, our aim is to better understand the biology of this disease and improve outcomes for patients.”
The NIH grant is project number 2 U01 NS100610-06.
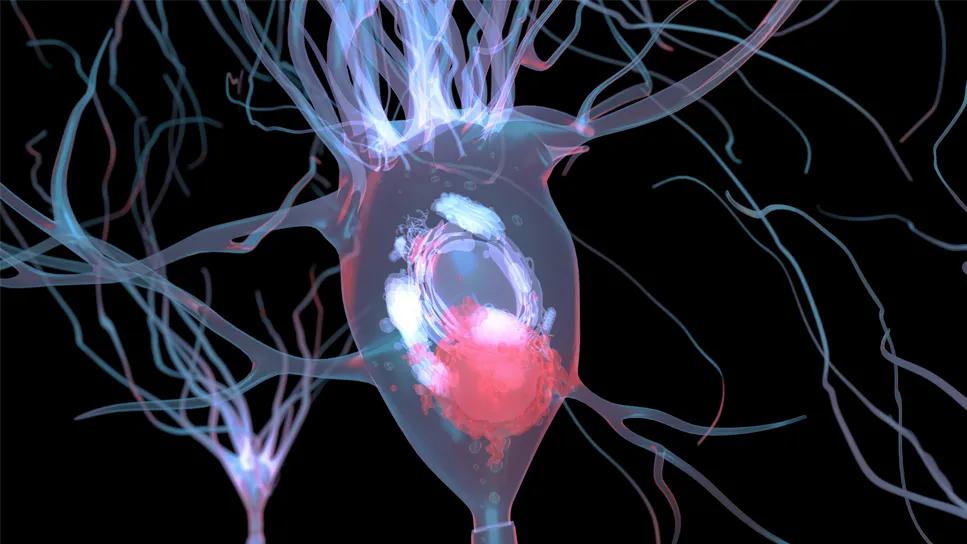
Pathology image at top shows a Lewy body inclusion (arrow) in a pigmented neuron of the substantia nigra.
Advertisement
Advertisement
GFAP elevation may signal increased risk of progressive regional atrophy, cognitive decline
Diagnosis and treatment of MOG antibody-associated disease

Model of viral encephalomyelitis shows links with CNS recovery from inflammation and damage

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Large NIH-funded investigation is exploring this understudied phenomenon

Initial results show good accuracy of scalable, low-cost tool for flagging cognitive decline

Novel insights from a postmortem study combining imaging, pathology and clinical perspectives

A principal investigator of the landmark longitudinal study shares interesting observations to date