Study reveals heavy care burden, missed opportunities in patients with uncontrolled symptoms on oral therapy

Device-aided therapy appears to be underused in patients with advanced Parkinson’s disease (PD) whose symptoms are poorly controlled with oral therapy, resulting in a high healthcare burden. So concludes a multicenter study that used the MANAGE-PD validated tool to assess patients with PD based on symptom control and eligibility for advanced treatment. The study was published in Parkinsonism & Related Disorders.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Patient and care partner satisfaction with treatment clearly is low across all MANAGE-PD categories and even lower for those in category 3,” says the study’s lead and corresponding author, Hubert Fernandez, MD, Director of Cleveland Clinic’s Center for Neurological Restoration. “Our findings highlight the value of identifying patients whose symptoms aren’t optimally managed and who may be candidates for device-aided therapy.”
Real-world data were prospectively collected between 2017 and 2020 from the Adelphi Parkinson’s Disease Specific Programme, a point-in-time survey of people with PD and their neurologists in seven nations (France, Germany, Italy, Japan, Spain, the United Kingdom and the United States). More than 2,700 patients on oral therapy for PD but naïve to device-aided therapy — defined as therapies such as deep brain stimulation, continuous infusion of levodopa/carbidopa intestinal gel or continuous subcutaneous apomorphine infusion — were included.
Using the MANAGE-PD tool, patients were grouped into three categories based on how controllable their PD symptoms were:
To identify treatment gaps and unmet patient needs according to patient categories, the investigators analyzed the dataset for the presence of motor symptoms, annual rate of PD-specific falls, need for assistance in activities of daily living (ADLs) and instrumental ADLs, PD-specific quality of life (QoL), care partner burden, patient and care partner satisfaction with current treatment, and whether patients and their care partners engaged in discussions about potential use of device-aided therapy.
Advertisement
Measures of healthcare resource utilization analyzed were the number of hospitalizations and emergency room (ER) visits in the prior 12 months, hours of professional care per week, whether a patient received respite care (to provide a short break for the primary caregiver), the number of healthcare provider consultations and scans for PD management in the prior 12 months, whether a patient’s care partners had stopped work or reduced work hours, and the number of different classes of PD drugs prescribed.
Comparisons between the three patient categories were made, with the investigators using regression analyses to adjust for age, sex, country and comorbidities.
Nearly half of patients (48.4%) were classified as MANAGE-PD category 1, 32.7% as category 2 and 18.9% as category 3. Patients in category 3 differed from their counterparts in the other two categories in several ways:
Analysis showed that patients in category 3 had significantly greater healthcare resource utilization than those in categories 1 and 2, including more hospitalizations, ER visits and consultations in the prior 12 months. They also were significantly more likely to have received respite care and be prescribed medications from a greater number of PD drug classes. Their care partners also were more likely to have stopped or reduced their work hours.
Advertisement
The most striking difference for category 3 patients was the number of hours of professional care required, which was 16-fold higher than for patients in category 1 (incidence rate ratio = 16.30; 95% CI, 8.72-30.46). “The scale of the differences in healthcare resource utilization was unexpected,” Dr. Fernandez notes. “The degree of burden compared with patients classified as category 1 or 2 was staggering.”
As expected, being in a higher MANAGE-PD category significantly increased the chances of discussing device-aided therapy with a provider. However, nearly half (45%) of patients in category 3 had never had such a discussion, which their care partners confirmed. “We found it surprising that in the advanced countries included in this study, where device-aided therapy is available and accessible, so many patients with advanced PD had not talked about it with their providers,” Dr. Fernandez observes.
The researchers conclude that these real-world data show that many patients continue with oral therapy alone despite insufficient symptom control and that these patients generally incur high healthcare resource utilization. They note that use of the MANAGE-PD tool may help identify these patients with greater treatment needs, and they issue a call to action for broader discussion of device-aided therapy among providers, patients and care partners alike.
The investigators emphasize that while device-aided therapy may be perceived as expensive, it compares favorably with the considerable cost of continuing on oral therapy that does not adequately control PD symptoms. “Not all patients with poorly controlled symptoms are candidates for device-aided therapy,” Dr. Fernandez concludes, “but raising awareness and involving all parties in treatment decisions may increase acceptance of it and lessen patient and care partner dissatisfaction with current treatment.”
Advertisement
Advertisement

Various AR approaches affect symptom frequency and duration differently

Dopamine agonist performs in patients with early stage and advanced disease

Early assessment could affect clinical decision making

Systems genetics approach sets stage for lab testing of simvastatin and other candidate drugs

Study aims to inform an enhanced approach to exercise as medicine

New tool for general neurologists aims to streamline differential diagnosis

When and how a multidisciplinary palliative care clinic can fill unmet needs for this population
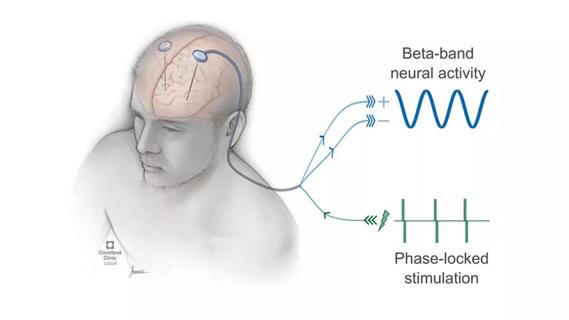
Research project will leverage insights into neural circuits to advance DBS technology