Despite advancements, care for this rare autoimmune disease is too complex to go it alone
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/14213903)
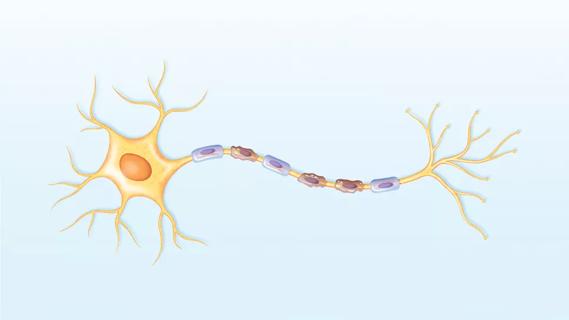
Neuromyelitis optica spectrum disorder (NMOSD), a rare demyelinating autoimmune disease predominantly affecting the spinal cord and optic nerves, was once thought to be a variant of multiple sclerosis (MS). That changed in 2004 with the discovery of the aquaporin-4 antibody (AQP4), a biomarker that explains the disorder’s pathogenesis. Now there are three FDA-approved treatments. However, patient management is complex and requires a team approach, says neuroimmunologist Justin Abbatemarco, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These are complicated cases,” explains Dr. Abbatemarco, a staff physician in Cleveland Clinic’s Mellen Center for Multiple Sclerosis. “Which sample do we send? Which antibody tests are best to use? NMOSD management is becoming more and more subspecialized, but don’t do it alone.”
In the latest episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Abbatemarco discusses diagnosis and management of NMOSD, including:
Click the podcast player above to listen to the 28-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
This activity has been approved for AMA PRA Category 1 Credit™ and ANCC contact hours. After listening to the podcast, you can claim your credit here.
Podcast host Glen Stevens, DO, PhD: Is there a prototypical phenotype with this patient population?
Dr. Abbatemarco: We think of three main kinds of clinical syndromes. One is optic neuritis, where the question is how to differentiate it from the typical optic neuritis we see in patients with MS. Severity is usually the differentiator — seeing severe vision loss in one or both eyes, 20/200 to even no light perception. When we’re looking at MRI, sometimes we can see optic chiasm involvement, which is very, very unusual in MS. So, bilateral optic nerve involvement, chiasm involvement, severe vision loss that doesn’t respond well to steroids and leaves people with permanent vision loss — these are all characteristics that are unusual in MS. So, severe optic neuritis in one or both eyes is a differentiator.
Advertisement
The next is transverse myelitis, and we usually characterize that as a longitudinally extensive transverse myelitis. So, greater than three vertebral body segments in length, usually involving the center of the cord, and causing severe disability. It’s important to note, however, that 15% to 20% of the spinal cord lesions in AQP4-positive NMOSD can be short segments. So, it doesn’t always have to be longitudinally extensive, but that’s something that is characteristic of NMOSD and is unusual in MS or other demyelinating diseases.
The third is area postrema syndrome, which is very unique to AQP4 disease. It causes intractable nausea, vomiting or hiccups. When you’re trying to tease that out in clinic, it’s a hard thing to ask about because everyone has experienced that. But what distinguishes it in NMOSD is having symptoms that last hours to days, usually requiring some kind of acute care management involving hydration or IV medication treatment.
Those are the three main clinical syndromes that we see, and it helps to think about them when we’re contrasting a specific patient’s clinical profile against MS attacks. There are other findings that we may see, but they’re much less common.
Advertisement
Advertisement

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

It’s time to get familiar with this emerging demyelinating disorder

From dryness to diagnosis
Early experience with the agents confirms findings from clinical trials
Treatment for scleroderma can sometimes cause esophageal symptoms
Patient’s symptoms included periorbital edema, fevers, weight loss

Could the virus have caused the condition or triggered previously undiagnosed disease?
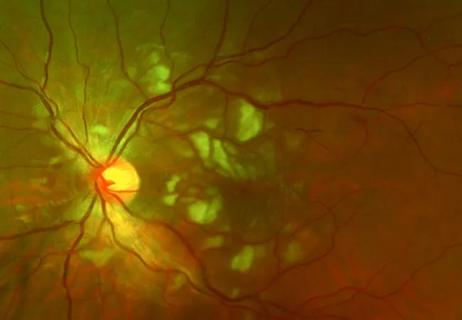
Good visual recovery and retinal reperfusion after prompt diagnosis and intensive therapy