Early experience with the agents confirms findings from clinical trials
In one of the first reports of real-world use of novel monoclonal antibodies (MAbs) for neuromyelitis optica spectrum disorder (NMOSD), the agents replicated the high rates of efficacy and safety observed in the randomized clinical trials that supported their FDA approval. So reported Cleveland Clinic researchers at the recent 2024 Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) Forum.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The observational study revealed good efficacy will all three novel MAbs studied — eculizumab (Soliris®), satralizumab (Enspryng®) and inebilizumab (Uplizna®) — and no serious adverse events. “Our findings provide reassurance to patients with NMOSD and their clinicians that good disease control and tolerability are highly likely if they start these treatments,” says the study’s senior author, Amy Kunchok, MD, PhD, of Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research.
The three novel MAbs studied were approved by the FDA in 2019 and 2020, becoming the first therapies indicated for the treatment of patients with aquaporin-4 immunoglobulin G-positive (AQP4-IgG) NMOSD. Despite robust clinical trial evidence of these agents’ safety and efficacy leading to their approval, data on their real-world use has been scarce.
“We wanted to look at these therapies outside of clinical trial conditions, as trials can be highly selective and tend to overrepresent patients who are healthier, more motivated and less disabled than the patient population as a whole,” Dr. Kunchok says. “Since Cleveland Clinic cares for a sizeable cohort of patients with NMOSD, we were well positioned to share our real-world experience with these therapies.”
She and colleagues analyzed data on all patients with AQP4-IgG NMOSD treated at Cleveland Clinic with a monoclonal antibody — one of the three novel MAbs or rituximab, which does not have regulatory approval to treat NMOSD — for more than 30 days.
Advertisement
Of the 104 patients included, 71 received rituximab and 33 received one of the newer agents— inebilizumab in 14, satralizumab in 12 and eculizumab in 7.
Median patient age was 58 and did not differ significantly between patients taking rituximab and those taking novel MAbs. Median baseline Expanded Disability Status Scale score was 4.75 and was also statistically comparable between the rituximab and novel MAb groups. A majority of patients in the novel MAb groups had received prior therapies, although some were treated with novel MAbs de novo.
Follow-up after the start of therapy was longer in the groups receiving rituximab and eculizumab (4.0 and 3.7 years, respectively) than in the groups receiving inebilizumab and satralizumab (1.3 and 1.1 years, respectively).
Key findings included the following:
Dr. Kunchok notes that the study is limited by its relatively short follow-up and the differences in duration of follow-up between rituximab and two of the novel MAbs. To address that, her group continues to follow this cohort and plans to report longer-term results in a future journal publication. They also are considering an analysis of how patients fared after switching to a novel MAb from other therapies.
Despite the current study’s limited follow-up, Dr. Kunchok says these preliminary findings so far support first-line use of the novel MAbs for patients with NMOSD when there are not insurance constraints to their use.
Advertisement
“We are encouraged that this real-world study has confirmed the clinical trial evidence behind the novel MAbs,” Dr. Kunchok concludes. “It is important for patients with NMOSD to have highly effective therapies to prevent relapses because we know that NMOSD-related disability is closely linked to the devastating relapses this disease can cause.”
Advertisement
Advertisement

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

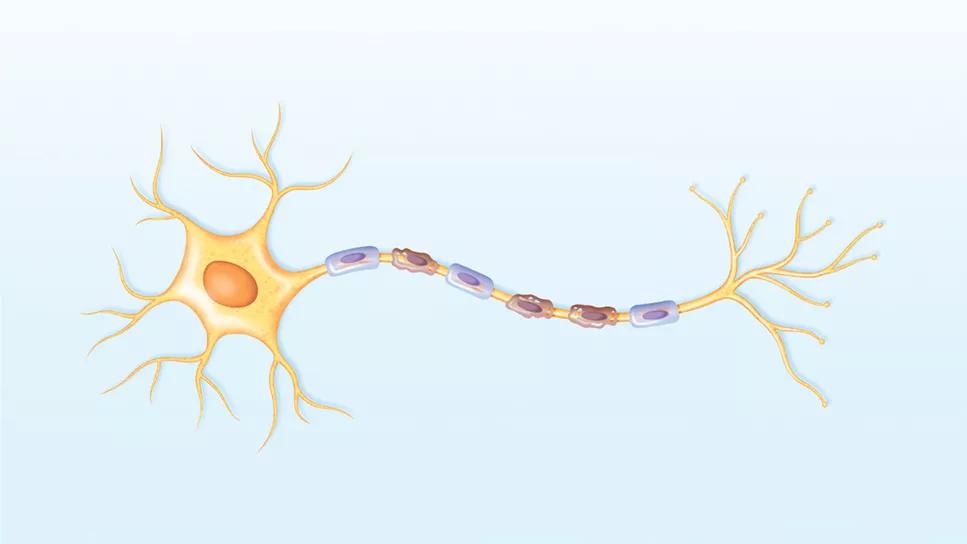
It’s time to get familiar with this emerging demyelinating disorder

From dryness to diagnosis

Despite advancements, care for this rare autoimmune disease is too complex to go it alone
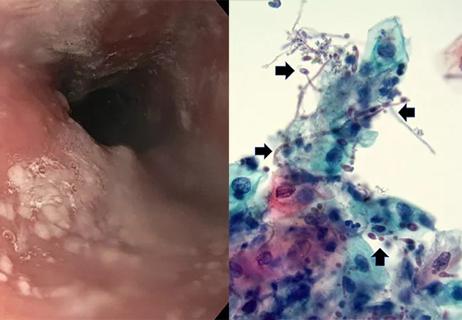
Treatment for scleroderma can sometimes cause esophageal symptoms
Patient’s symptoms included periorbital edema, fevers, weight loss

Could the virus have caused the condition or triggered previously undiagnosed disease?
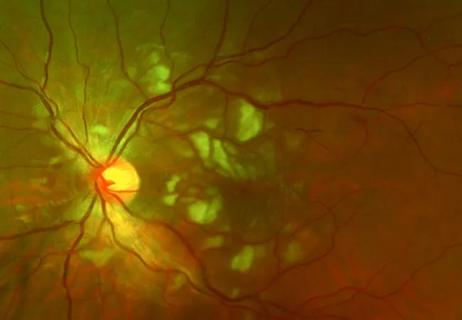
Good visual recovery and retinal reperfusion after prompt diagnosis and intensive therapy