An uncommon condition in a 41-year-old man
By Soumya Chatterjee, MD, MS, FRCP
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A previously healthy, 41-year-old man presented to our clinic with diffuse skin thickening on his arms, legs and abdomen and a history of myalgias. About 12 months before coming to clinic, the patient experienced a flu-like illness accompanied by ankle swelling and a feeling of skin tightening in the inner aspects of his thighs and legs, the antecubital fossae, chest and abdominal wall.
He attributed myalgias and an 18-pound weight loss to vigorous exercise but ceased running and lifting as symptoms progressed and joint contractures developed, including elbow contractures that left him unable to fully extend his arms. He denied joint pain and swelling but reported some joint stiffness and muscle weakness. He denied the use of athletic supplements, tobacco and alcohol, and did not appear to have dysphagia, digital pits or ulcers, dyspnea, dysphagia, fever or cough. He took 40 mg omeprazole daily for chronic heartburn.
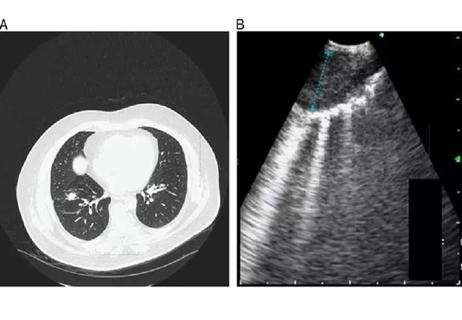
The skin of his upper arms, forearms, lower abdomen, inner thighs and lower legs all showed an orange peel-like appearance (figure A). No tendon friction rubs, sclerodactyly or puffiness in the hands were present. Clinical evidence of proximal myopathy was lacking despite some limitations in shoulder range of motion. Veins furrowed along the superficial veins of his forearm (figure B). Heart and lung examinations and nail-fold capillaroscopy were normal.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a35c31c8-0fc8-4f1b-be80-abb40f8a21eb/18-RHE-1031-Chatterjee-Hero-Image-650x450pxl_jpg)
(A) Skin induration with a peau d’orange appearance in the right arm of a 41-year-old man with a one-year history of skin tightening. (B) Furrows along the superficial veins of the patient’s raised right forearm. Republished with permission from the Canadian Medical Association.
Advertisement
We considered a few conditions for this patient:
The location and appearance of the patient’s skin induration were not characteristic of Type 1 or 2 of scleredema, so we eliminated choices 3 and 5. We also deemed choice 1 unlikely given the lack of Raynaud phenomenon, digital ulcers or pits, sclerodactyly, nail-fold capillary abnormalities and tendon friction rubs. Without a history of chronic kidney disease or known exposure to gadolinium-based contrast agents, choice 4 became highly unlikely. A recent uptick in vigorous exercise, the vein furrows and orange-peel skin are all important clues to this diagnosis.
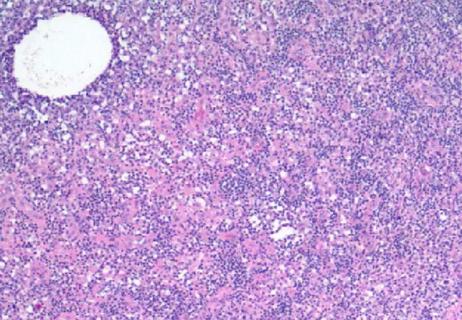
To confirm a diagnosis of our remaining choice, diffuse fasciitis with eosinophilia, we ordered a full-thickness skin biopsy including subcutaneous fat, fascia and underlying muscle. Standard labs were unremarkable. (Click here for a table of key features on skin biopsy in the main diffuse sclerosing skin conditions). The biopsy confirmed his diagnosis. We prescribed 60 mg daily prednisone with a taper to 5 mg daily. The addition of 200 mg hydroxychloroquine twice daily further reduced his symptoms within six months. Our patient has not developed hematologic malignancies, which occur in about 10 percent of patients.
Diffuse fasciitis with eosinophilia is uncommon, and its exact etiology is unknown. Case reports show intense exercise, trauma, chronic cutaneous graft-versus-host disease, drug exposures, bug bites and Borellia burgdorferi infection as possible triggers.
Advertisement
This patient’s case followed the common progression of the disease, which I and my colleague Richard Prayson, MD, MEd, Section Head of Anatomic Pathology, describe in detail in our case report published in the Canadian Medical Association Journal.
Diagnosing diffuse fasciitis with eosinophilia involves lab testing, MRI and physical and histopathologic examination. Patients can develop elevated inflammatory markers, polyclonal hypergammaglobulinemia and eosinophilia; however, eosinophilia is not required for diagnosis given its rapid resolution with the start of therapy. MRI will show fascial inflammation.
Definitive diagnosis requires a full-thickness incisional biopsy from skin to muscle. Findings typically include histiocytes, mast cells and eosinophils infiltrating the deep dermis, fascia and superficial muscle but usually sparing the epidermis, papillary dermis and adnexa. Lymphoplasmacytic inflammation is present, and sclerosis and fibrosis thicken the deep fascia.
Glucocorticoids (GCs) in moderate to high doses are the standard therapy for diffuse fasciitis with eosinophilia. Patients should take great caution with exercise and should be monitored for hematologic malignancies. Hydroxychloroquine or methotrexate can augment therapy if GCs are inadequate.
This case demonstrates the importance of understanding the differentiating features of the diffuse sclerosing skin conditions.
Dr. Chatterjee directs the Scleroderma Program in the Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement
Advertisement

Screen patients seeking care for chlamydia, gonorrhea

Lingulectomy removes infection when antibiotics fail

Researchers have developed immunoprofiles for an emerging disease with a mortality rate as high as 27%

Findings from one of the first published case series
Don't discount this crucial step
EBUS-TBNA found safe and effective
How to spot the rare infection

Not all lung nodules are malignant