A promise of solutions where traditional MEG falls short
By Balu Krishnan, PhD, and Andreas Alexopoulos, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Accurate localization of the epileptogenic focus in patients with intractable epilepsy has a positive impact on the long-term outcome of resective surgery. As part of our continuous effort to improve surgical outcomes, Cleveland Clinic’s Epilepsy Center initiated new research to investigate the use of resting-state magnetoencephalography (MEG) data to localize epileptogenic foci.
MEG offers a direct measurement of whole-brain neuronal activity while preserving high spatial and temporal resolutions. Traditional MEG-based analyses in epilepsy have relied on source modeling of epileptiform activity. The study pioneered by our neurophysiology team relies on noninvasive localization of the epileptic focus based on analysis of resting-state directional connectivity of the epileptic brain (in this case, resting state means that no epileptiform discharges are necessary) using advanced signal processing of MEG data. This approach is based on the premise that the epileptic focus has increased information exchange from neighboring neural structures during the resting state.1,2
Our pilot study on the use of resting-state MEG data for localization of epileptogenic foci was funded by an American Epilepsy Society Young Investigator Award. The study analyzes resting-state MEG recordings from 22 consecutive patients with medically refractory epilepsy who underwent resective surgery and have been seizure-free for at least one year. Information transfer between different brain regions was estimated using techniques from Granger causality. Graph theoretical centrality measures were used to identify important nodes of the connected network, and an asymmetry index was employed to quantify the degree of bilateral asymmetry in graph theoretical measures. Concordance with the epileptogenic zone was evaluated by comparing the regions of high asymmetry with those of the resection cavity. Connectivity-based investigation was able to identify the epileptogenic zone in 16 of the 22 patients, including eight patients in whom localization was not possible via traditional MEG analysis due to the absence of an adequate number of interictal abnormalities.
Advertisement
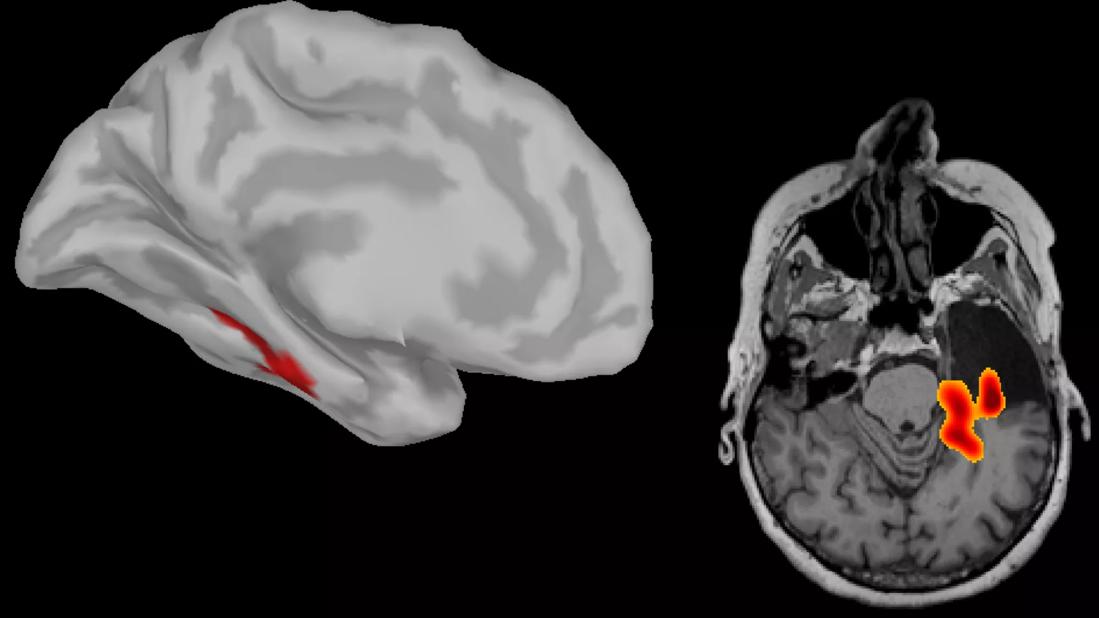
The figure below shows the net information exchange into (panel A) and out of (panel B) insular cortex across 22 patients. Panel C shows findings from a patient who underwent right temporal lobectomy. A high asymmetry index in network centrality can be observed in the left mesial temporal lobe. Panel D presents an example of where a high asymmetry index in network centrality was observed in the right middle frontal gyrus and the left lingual area (not shown). This patient underwent resection of the right middle frontal gyrus and has been seizure-free.
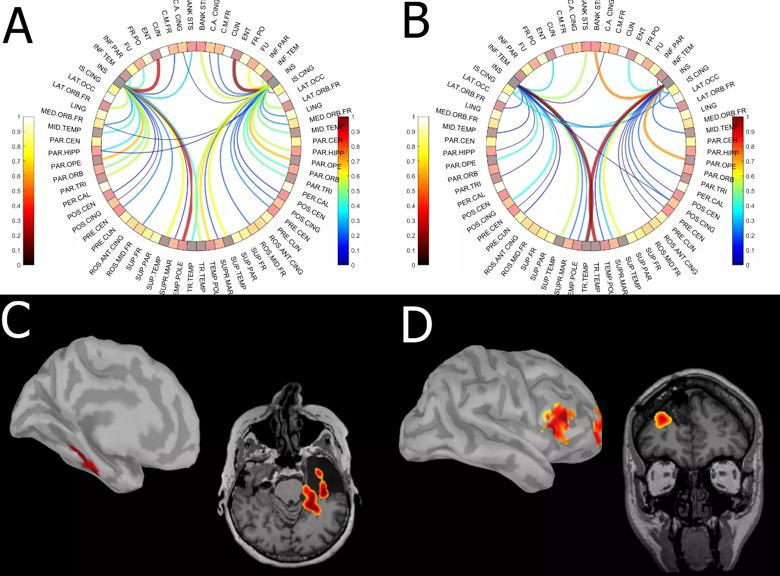
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c1ff4988-1324-4874-9f1c-b0493805f7a0/Krishnan-inset_png)
Figure. Average information exchange map for insular cortex across 22 patients. Panel A shows net information exchange to insula from other cortical regions, whereas panel B shows net information exchange from insula to other cortical regions. Panels C and D present illustrative examples of results of focus localization using resting-state connectivity analysis rendered of patients’ individual cortex and postoperative MRI. Panel C shows a case of temporal lobe epilepsy in which high connectivity was observed in the left hippocampal formation. The patient underwent left temporal lobectomy. Panel D shows a case of frontal lobe epilepsy in which high connectivity was observed in the left lingual (not shown) and right middle frontal gyrus. The patient underwent resection of the right middle frontal gyrus and has been seizure-free. See text for additional discussion.
Our results provide evidence that noninvasive resting-state data carry important information regarding the pathophysiology of epilepsy and could guide therapeutic targeting to improve patient care. The connectivity-based technique has conceptual advantages over traditional point-based models in that it does not rely on the presence or absence of epileptiform abnormalities during MEG acquisition. This critical advantage of resting-state technique can contribute to the yield of MEG studies by providing solutions to MEG-negative cases (i.e., those with an absence of epileptic events).
Advertisement
Traditionally, whole-brain functional connectivity analysis has been performed using functional MRI. Functional MRI studies rely on measurement of hemodynamic changes, which fluctuate at a slower time scale relative to neural activity. The superior temporal resolution of MEG can be useful in the estimation of directional connectivity measures from the neural activity. As a result, resting-state MEG analyses can be used to investigate brain networks, paving the way for applications that go beyond epilepsy to address the role of networks in other neurological diseases (e.g., dementias), cognitive conditions (e.g., autism) and psychiatric conditions (e.g., schizophrenia, depression, anxiety).
Dr. Krishnan is a research scientist in Cleveland Clinic’s Epilepsy Center.
Dr. Alexopoulos is a staff physician in the Epilepsy Center.
Advertisement
Advertisement

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant