Phase 3 EXPAND trial suggests potential utility of siponimod
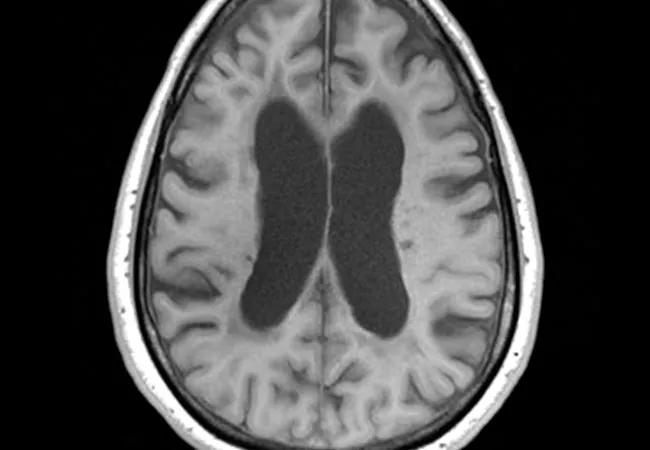
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/efa664e3-a488-4169-81e4-c0e58c84a16e/18-NEU-678-Progressive-MS-650x450_jpg)
18-NEU-678-Progressive MS-650×450
For the first time, a disease-modifying therapy for secondary progressive multiple sclerosis (SPMS) has shown superiority over placebo in slowing patients’ disability progression in a large randomized trial. So report investigators with the multicenter phase 3 EXPAND trial of siponimod, an investigational oral sphingosine-1-phosphate (S1P) receptor modulator, newly published in The Lancet.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is an important finding, because no drug has yet consistently slowed disability progression in patients with the secondary progressive form of MS,” says study co-author Robert Fox, MD, a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis Therapy and Research, which was among the EXPAND trial’s participating sites. “These results suggest that siponimod may be a useful treatment for secondary progressive MS, although longer-term follow-up and regulatory approval is needed.”
Siponimod is believed to act by decreasing inflammation and preventing synaptic neurodegeneration and/or promoting remyelination in the CNS.
The double-blind EXPAND study randomized 1,651 patients from 31 countries on a 2:1 basis to siponimod 2 mg orally once daily or placebo for up to three years or until their disability had progressed after six months. Participants whose disability progressed were offered open-label siponimod.
Patients were 18 to 60 years old and had moderate to advanced disability (Expanded Disability Status Scale [EDSS] score of 3.0 to 6.5). Baseline mean MS duration was 17 years and mean duration of SPMS was four years. Sixty-four percent of patients had not relapsed in the prior two years, and 55 percent required walking assistance.
Patient disability levels were assessed every three months, and brain MRIs were taken at baseline and at 12, 24 and 36 months.
Of the 1,651 patients randomized, 1,645 were included in the analysis (1,099 randomized to siponimod and 546 to placebo). Study completion was achieved by 82 percent of the siponimod group and 78 percent of the placebo group. Eleven percent of placebo recipients switched to open-label siponimod after confirmed disability progression at six months.
Advertisement
The study’s primary end point — confirmed disability progression at three months — was reached by significantly fewer siponimod recipients (26 percent) compared with placebo recipients (32 percent), for a risk reduction of 21 percent (hazard ratio = 0.79; 95% CI, 0.65-0.95 [P = .0134]) with active treatment. Siponimod also showed a statistically significant 26 percent relative risk reduction in confirmed disability progression at six months, a secondary end point.
On other secondary outcome measures, although siponimod had no significant effect on maintenance of walking speed (as assessed by timed 25-foot walk test), it significantly reduced the increase in T2 lesion volume on MRI from baseline to 24 months compared with placebo. “Loss of brain volume is an important marker for tissue damage in MS,” Dr. Fox explains.
Adverse events occurred at a modestly higher rate in siponimod recipients than in placebo recipients (89 vs. 82 percent), as did serious adverse events (18 vs. 15 percent). Early dose titration attenuated first-dose cardiac effects. Rates of infections, malignancies and death did not differ between the groups. Siponimod’s safety profile appears to be similar to that of other S1P receptor modulators, the study authors observed.
Dr. Fox notes that while the 6 percent absolute reduction and 21 percent relative reduction in the risk of three-month disability progression with siponimod may seem modest, “even numerically small changes in EDSS score can correspond to substantial changes in neurological function and daily activities for patients with secondary progressive MS.”
Advertisement
The study report points out that enrollees’ previous therapies may have affected their response to siponimod. An additional limitation is that patients randomized to placebo who elected to receive open-label siponimod after disability progression were included in the efficacy analysis, potentially reducing siponimod’s effect size on some secondary outcomes. A study strength is its very large population of typical SPMS patients with characteristics compatible with other studies in SPMS and natural history data, the authors note.
“Overall, the results of this trial support that siponimod may be a useful treatment for patients with SPMS,” the researchers conclude, adding that “further more sophisticated analyses and longer-term observations are underway” that may help further define the agent’s potential utility.
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges