Largest real-world cohort of polycythemia vera patients
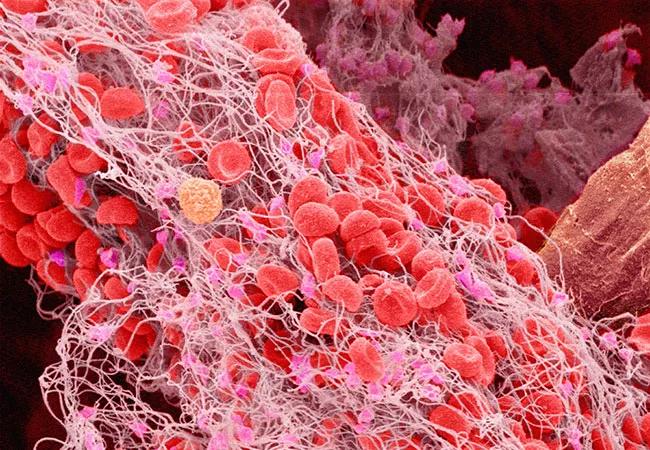
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/aeda1813-69e6-438c-a56a-794b8248be93/22-CNR-2932808-CQD-Hero-650x450-1_jpg)
22-CNR-2932808-CQD-Hero-650×450
A strong connection exists between elevated blood counts and increased thrombotic event risk in patients with polycythemia vera, according to research results presented at the 2022 European Hematology Association meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A link between elevated hematocrit (red blood cell counts) and thrombosis has been long-established. As part of a nationwide study, researchers at Cleveland Clinic found that patients with elevated white blood cell count or platelet count also experienced higher incidents of thrombotic events such as blood clots, acute myocardial infarction and deep vein thrombosis. Notably, an elevated white count (>12) is significantly associated with increased risk of thrombotic events when hematocrit is controlled, indicating that risk factors may be reduced by controlling white blood cell count as well as hematocrit.
Blood clots are a leading cause of morbidity and mortality in patients with polycythemia vera, yet there is still much to learn about the risk factors for these thrombotic events. “Just assessing risk based on age and prior history of blood clots is a very crude tool,” says study co-author Aaron T. Gerds, MD, MS, a staff physician with Cleveland Clinic Taussig Cancer Institute and Associate Professor of Medicine (Hematology and Medical Oncology) with the Cleveland Clinic Lerner College of Medicine. “Understanding what causes these patients to have blood clots is the first step in intervening on a deeper level to prevent clots from occurring.”
While the connection between thrombotic events and elevated hematocrit levels has been well documented, the association between higher platelet and white blood cell counts had not been evaluated in a consistent manner. Researchers sought to better understand these associations to develop more effective risk stratification.
Advertisement
To determine whether increased blood counts are predictive of thrombotic events, Dr. Gerds and his colleagues analyzed data from the REVEAL study, which is the largest prospective observational study about patients with polycythemia vera. They evaluated records for patients who had adequate numbers of blood counts recorded in the database. Of those 2,271 patients, 30 had arterial thrombotic events and 76 had venous thrombotic events. Among the 456 patients with a previous thrombotic event, 38 experienced another such event during follow-up.
“As the white blood cell count increases, we see increasing risk of blood clots,” says Dr. Gerds. “The association between elevated platelets is a little less clear. We did see an increased risk with elevated platelets, but when you raise the threshold to 600, there is no longer an association between platelet count and blood clot risk.”
The association between blood count levels and thrombotic events was assessed using a time-dependent covariate Cox proportional hazards model. Time to first post-enrollment thrombotic event was modeled with follow-up time censored at last known visit for patients without a thrombotic event. Blood counts at the last lab test prior to thrombotic event or end of follow-up were included as binary time-dependent covariates using the established thresholds of hematocrit >45%, white blood cell count >11 and platelet count >400. Alternative thresholds of white blood cell count <7; ≥7 to <8.5, ≥8.5 to <11 ≥11 and platelet count >600 were also evaluated.
Advertisement
Under conditions where hematocrit was controlled, the association between white blood cell count elevation >11 did not quite reach significance. However, use of a higher white blood cell count threshold of >12 resulted in a significant association between elevated white blood cell count and thrombotic event risk.
The data supports the notion of incorporating blood count values into risk stratification and treatment strategies for patients with polycythemia vera.
Dr. Gerds noted that this is the first step in a long process of data analysis. The researchers are now delving further into REVEAL study data to assess the relationship between thrombotic event risk and isolated white blood cell count elevation, as well as time-dependent risk with elevated blood count.
“We need to validate that elevated white blood cell count is a risk factor for thrombosis,” says Dr. Gerds. “And more importantly, we need to demonstrate that by lowering white blood cell count we can reverse the increased risk of thrombosis. Conversely, identifying those at lower risk may allow for the use of less aggressive treatments in those cases. Doing so would have a tremendous impact on clinical practice.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches