Large single-center series details outcomes of several advanced interventions
Critically ill patients with uncontained esophageal perforation have several advanced therapy options, from esophageal repair to esophagectomy and complete alimentary tract diversion with the possibility of eventual reconstruction for the most severe cases. Advanced interventions — and characteristics of 166 patients on whom they were performed at Cleveland Clinic — were recently described in the Annals of Surgery (2021;274[5]:e417-e424). The report, which covers cases over a 20-year period, represents the largest single-institution series of advanced intervention for esophageal perforations published to date.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“With more options available, the paradigm for treating esophageal perforation has changed over the years, as have outcomes,” says the paper’s senior author, Sudish Murthy, MD, PhD, Section Head of Thoracic Surgery at Cleveland Clinic. “Despite severe illness, even patients requiring esophageal diversion can now benefit from operative intervention, with excellent long-term survival.”
Esophageal perforation is often fatal without invasive intervention. Because of its rarity and heterogeneous etiology and presentation, optimal management strategies have not been well defined.
This study was designed to characterize patients who underwent an advanced intervention for esophageal perforation at Cleveland Clinic to identify factors associated with therapy decisions and treatment outcomes.
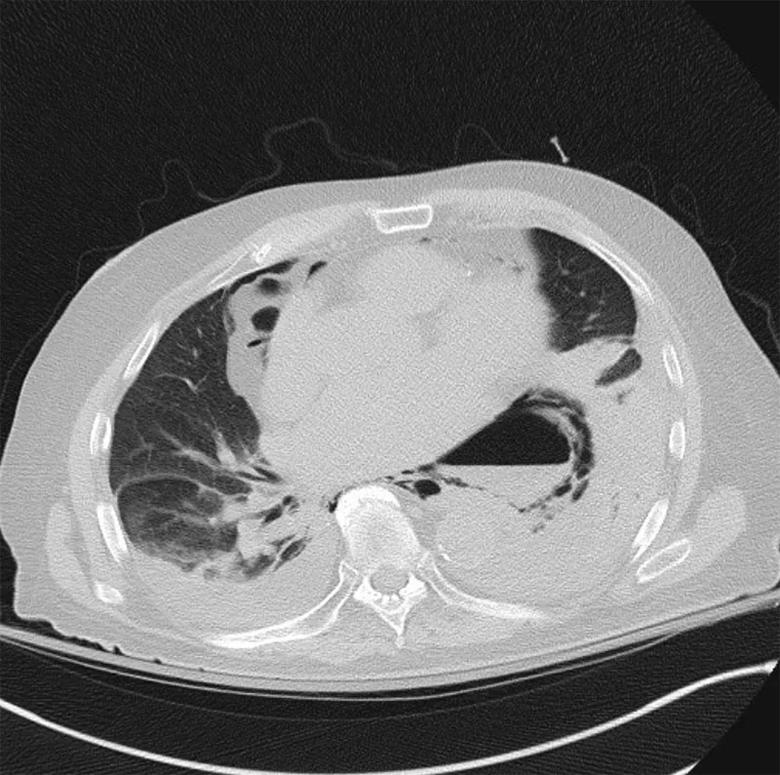
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1caac4b0-ccbc-4e74-9b1d-3c3a4653593a/21-HVI-2549309-inset-perforated-esophagus-800x795-1_jpg)
CT scan showing an esophageal perforation.
Patients who had an esophageal perforation managed by advanced surgical intervention at Cleveland Clinic from 1996 to 2017 were included in the study (N = 166; mean age, 61 ± 16 years; 54% female).
The following interventions were performed:
Advertisement
Illness severity was retrospectively quantified using the Pittsburgh Severity Score (PSS; range, 0-18), which takes into account risk factors at presentation that are associated with mortality (i.e., age, tachycardia, leukocytosis, pleural effusion, fever, uncontained leak, respiratory compromise, time to diagnosis, cancer, hypotension). A validation study from another institution found that a score over 5 is associated with an in-hospital mortality rate of about 40%.
The mean PSS in the entire cohort was 5.0 ± 3.3; 25% had a PSS > 7. Mean PSS was 3 points for both the repair and resection groups versus 6 points for the resection-diversion group (P = 0.002).
Outcomes following interventions were as follows:
Risk of death following resection-diversion was highest within the first year. However, 52% of patients with this intervention went on to undergo reconstruction of the upper alimentary tract within two years.
“The risk of death was high for the most severe cases during the first year, but for those who survived this period and underwent reconstruction, survival was excellent,” Dr. Murthy says.
Severity of disease at presentation should determine treatment, the study authors emphasize. Dr. Murthy notes that the PSS is a reasonable method for assessing severity and can help guide intervention and management, although other factors also must be considered.
Advertisement
At one end of the spectrum, patients with a small contained perforation often can be managed expectantly, and endoscopic stent placement plus pleural drainage may be sufficient even for full-thickness perforations if soilage is limited.
For more severe presentations and for patients who do not respond to nonoperative management, the authors recommend the following general strategy for advanced intervention:
“Repair and organ preservation are always preferred, if possible,” observes study co-author Siva Raja, MD, PhD, of the Section of Thoracic Surgery. “However, extensive mediastinal and pleural soilage, in addition to hemodynamic instability, often make this impractical.” In such cases, he says, resection-diversion can be an important life-saving option.
Advertisement
“Despite advances in minimally invasive and endoscopic surgery, life-threatening problems like esophageal perforations sometimes require big operations to start, as we may not have a second chance to salvage critically ill patients,” Dr. Raja concludes. “Studies such as ours can provide guidance to surgeons who are debating between the various options to treat esophageal perforations based on the clinical picture.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more