Recurrences were rare and survival robust in large Cleveland Clinic study
Most patients who undergo resection of benign primary cardiac tumors can be considered “cured,” concludes a large database study from Cleveland Clinic researchers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We found that surgical resection of these tumors yields excellent outcomes,” says Eric Roselli, MD, a Cleveland Clinic cardiothoracic surgeon and senior investigator on the study, presented at the recent 60th annual meeting of the Society of Thoracic Surgeons. “In patients with myxomas, the procedure restores survival to a level observed in a matched general U.S. population.”
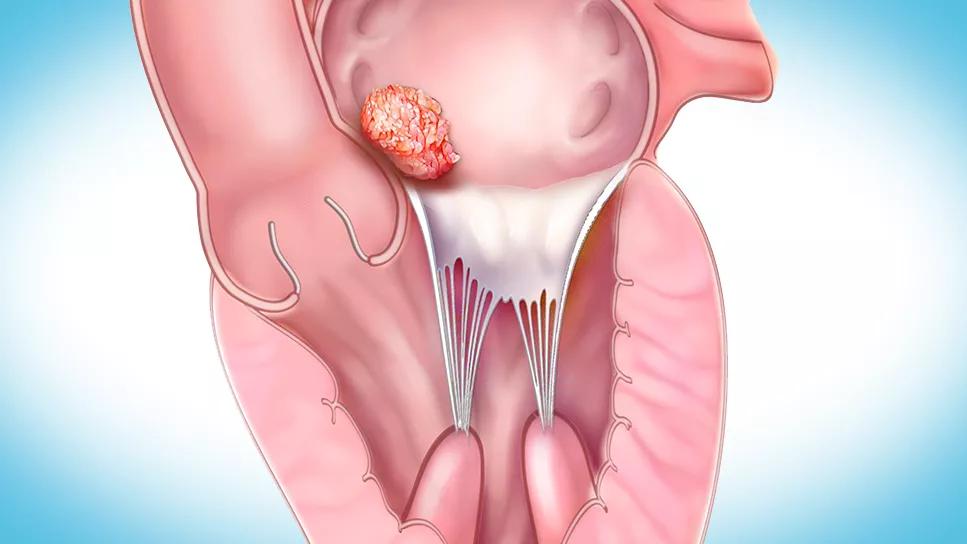
With a prevalence of no more than 0.3% in autopsy series, primary cardiac tumors are rare. Most are benign and carry a good prognosis, but they can have hemodynamic and arrhythmic implications for patients.
Surgical resection remains the preferred treatment for primary cardiac tumors, but few studies have been done in patients undergoing resection. Recently, Cleveland Clinic researchers published a retrospective analysis of outcomes after resection of malignant primary cardiac sarcoma over a 35-year period (JTCVS Open. 2021;8:384-390). In the new study, these investigators have assessed early and late survival and recurrence after resection of benign cardiac tumors.
“This may be the largest reported experience with surgical resection for benign cardiac tumors at a single institution,” Dr. Roselli notes. “Over nearly six decades, we observed only two tumor recurrences among more than 500 patients. This confirms that good long-term results are achievable for almost all patients, although careful and complete surgical excision is likely crucial to these outcomes.”
The researchers analyzed surgical resections of benign primary cardiac tumors performed on 563 patients at Cleveland Clinic from 1965 through 2022. The vast majority of tumors were myxomas (62%) or papillary fibroelastomas (30%), with the remainder consisting of rare tumor types including lipomas (2.8%), paragangliomas (1.8%), fibromas (0.9%) and hemangiomas (0.9%).
Advertisement
Data about patients, whose diagnoses were all confirmed histopathologically, were taken from Cleveland Clinic’s Cardiovascular Information Registry as well as medical records and follow-up surveys. Mean age at resection was 59.2 years in the patients with myxomas, 64.9 years in patients with papillary fibroelastomas and 54.4 years in those with other rare tumors. Other data captured included history of cardiovascular disease, postoperative complications and concomitant surgical procedures, which were done in 35.5% of the myxoma group, 73.4% of the fibroelastoma group and 55.6% of the other rare tumor group — most commonly valve procedures.
Intracardiac tumors were left-sided in 92% of myxomas, 81% of papillary fibroelastomas and 56% of rare benign tumors. The left atrium was the location of most of the myxomas (89%), whereas fibroelastomas occurred at various sites, including the aortic valve (38%) left atrium (20%) and left ventricle (19%). The rare tumors were found in the right atrium (29%), left atrium (24%), left ventricle (24%) and right ventricle (18%).
The analysis revealed a generally steady increase in the prevalence of benign cardiac tumors over the study period, with the largest increases seen after the year 2000. “We found an increased prevalence over time, which may be a result of improvements in noninvasive diagnostic tools,” observes cardiothoracic surgery research fellow Annalisa Bernabei, MD, who presented the study findings.
There were 10 operative deaths (1.8%), six of which occurred after major concomitant procedures and two in cases involving extensive tumors during an earlier period in the study.
Advertisement
Median duration of follow-up was 4.5 years, with 25% of patients followed for more than 12 years, 10% for more than 20 years and 5% for more than 25 years. Survival rates were as follows:
Survival was significantly higher (P < .001) in patients with cardiac myxomas than in patients with other tumor types. In fact, survival among patients with myxomas was comparable to that of the general U.S. population. “Patients with myxomas also were significantly less likely to undergo a concomitant cardiac procedure, which may explain why their survival was better,” Dr. Roselli notes.
Two tumors — both left atrial myxomas — recurred during follow-up. New strokes occurred in five patients during follow-up — two in patients with myxomas and three in patients with fibroelastomas. The low incidence of stroke during follow-up is notable, the researchers observed, since 14% of the study population had a history of stroke at baseline.
“Despite the relative rarity of benign cardiac tumors, Cleveland Clinic is now performing 40 to 50 of these surgeries per year,” notes co-investigator Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery. “These results show that when these surgeries are performed at a high-volume center, the outcomes can be excellent in the short and long term. In addition, isolated myxomas and fibroelastomas can often be removed using robotic technology, which enables very small incisions.”
Advertisement
“This collated database is a wonderful resource for cardiologists to use as a benchmark for managing these infrequent cases, and to prompt referral to an experienced center so patients can benefit from surgical expertise that can realistically offer cure,” adds co-investigator Patrick Collier, MD, PhD, a cardiologist who co-directs Cleveland Clinic’s Cardio-Oncology Center. “At the best centers, that surgical expertise is provided after careful assessment and consideration by an integrated care team guided by precise, advanced imaging.”
Advertisement
Advertisement

‘Concise clinical guidance’ from ACC distills key advances in imaging and pharmacotherapy

First prognostic tool of its kind for a challenging, debilitating condition

Offers recommendations on imaging and treatment across five clinical pericardial syndromes

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR