Study supports addressing mitral regurgitation before mild tricuspid regurgitation progresses
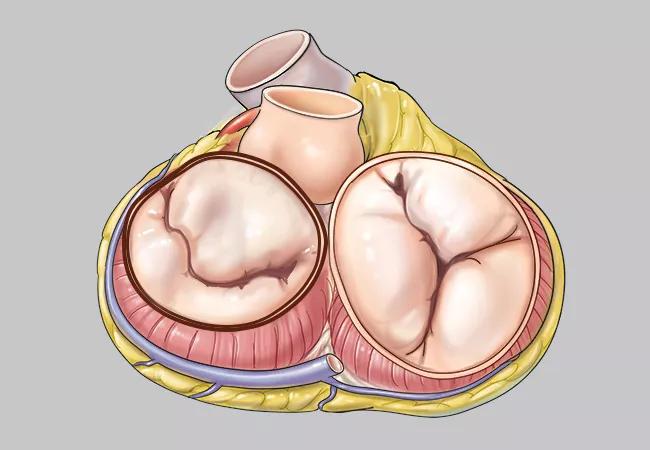
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5a1913fd-e9c7-429d-a6f7-8a410716e40f/22-HVI-2729215-CQD-650x450-1-jpg)
illustration of mitral and tricuspid valves of the heart
The presence of moderate tricuspid regurgitation (TR) at the time of isolated mitral valve (MV) repair for severe degenerative mitral regurgitation (MR) raises the long-term risk of incomplete resolution of the TR — and risk of death — compared with the absence of TR or the presence of only mild TR.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So finds a registry-based study of nearly 5,500 patients who underwent MV repair without concomitant TR intervention at Cleveland Clinic and were subsequently followed for up to 24 years. The study was published in JTCVS Open (2025 Epub 10 Apr).
“Although we hope that tricuspid regurgitation will resolve after the mitral valve is addressed in patients with severe degenerative MR, that doesn’t always occur, and it’s hard to predict which patients will gain this benefit,” says senior author Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “Because we observed a significant reduction in long-term survival in those with preoperative moderate TR, we conclude that offering mitral valve repair earlier in the course of degenerative mitral valve disease — before TR progresses beyond the mild stage — is advisable.”
Whether to address moderate TR at the time of MV surgery is unclear. A recent randomized trial from the NIH-funded Cardiothoracic Surgical Trials Network (CTSN) (New Engl J Med 2022;386:327-339) found that patients with severe degenerative MR and moderate TR who underwent MV repair and concomitant tricuspid valve repair had reduced TR progression at two years but had rates of mortality and readmission similar to those in patients with mild or no TR who underwent MV repair alone.
Dr. Gillinov, who serves as Chair of the CTSN, noted that initial follow-up in their NIH-funded trial extended to only one to two years. Therefore, the new Cleveland Clinic study was designed to characterize the natural progression of TR following MV repair and assess its impact on survival over a longer follow-up period.
Advertisement
This study included 5,467 patients (mean age, 58 years) with severe degenerative MR who underwent MV repair without concomitant TR repair from 2000 through 2022. At the time of repair, 3,418 patients (63%) had no TR, 1,652 (30%) had mild TR and 397 (7%) had moderate TR. Patients were followed for up to 24 years (median follow-up for survival was 4.2 years [mean, 5.5 years]).
The group with preoperative moderate TR had more risk factors than patients with mild or no TR: They were older (mean age, 65 vs. 58 years), had more comorbidities (including atrial fibrillation/flutter, congestive heart failure, complete heart block/pacer and history of cerebrovascular events) and were likelier to be on renal dialysis. They also tended to have a larger left atrial volume index and higher right ventricular systolic pressure, and they were more likely to have undergone an atrial fibrillation procedure at the time of MV repair.
Principal findings of the study are summarized below.
Advertisement
The attenuation of the increased mortality risk in patients with preoperative moderate TR after risk-adjusted analysis suggests that this increased risk might have been attributable to a higher baseline risk profile, the study authors note.
“An unanswered question is whether the TR is primarily responsible for reduced survival or whether accompanying risk factors — such as older age and increased comorbidities — are to blame,” says Tarek Malas, MD, MPH, a Cleveland Clinic cardiothoracic surgeon and co-author of the study. “We couldn’t answer this from our study, but our findings do suggest that mitral valve intervention before a patient develops more advanced TR — and becomes older and sicker — appears to be a prudent strategy. That’s especially the case for patients with other risk factors, such as low left ventricular ejection fraction or elevated right ventricular systolic pressure.”
“Our goal is to operate on patients with severe degenerative mitral regurgitation before they develop TR,” Dr. Gillinov notes. “If patients have moderate or greater TR at the time of mitral valve surgery, a tricuspid valve repair should be added. Fortunately, with current technology, we can perform combined mitral valve and tricuspid valve surgery with incredibly low mortality (less than 0.1%) — and often with a robotic/minimally invasive approach.”
“This study indicates that moderate TR at the time of mitral valve surgery often reflects a higher burden of comorbidities and an overall sicker patient profile, and that it’s associated with worse long-term outcomes,” adds Cleveland Clinic cardiologist Serge Harb, MD, who was not involved in the study. “These findings support intervening on severe degenerative mitral regurgitation before TR progresses beyond the mild stage, and they underscore the importance of a collaborative heart team approach when considering the timing and extent of valve intervention.”
Advertisement
Advertisement
TRISCEND II trial reports 1-year results
Limited data and experience will translate to a cautious rollout
Cleveland Clinic study argues against waiting for symptoms to develop
TEER is found to be a safe and good option for severe TR in select patients
Understanding VC anatomy is critical for transcatheter tricuspid valve interventions
Scenarios where experience-based management nuance can matter most
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon