New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits
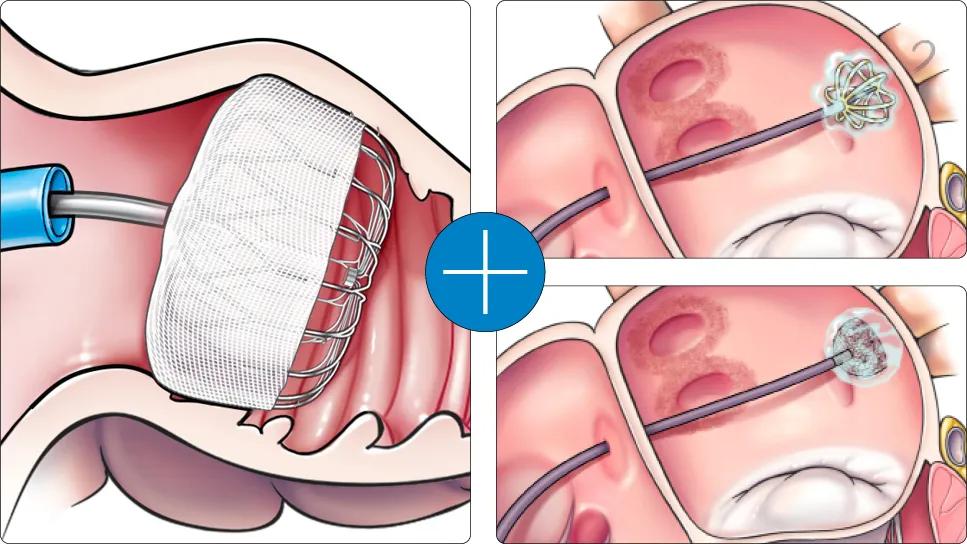
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1bce4cbc-5afe-40fb-9e4a-847755decb11/25-HVI-6702014-CQD-hero-957x544)
illustrations of two heart procedures connected with a plus sign
When primary results of the landmark multicenter OPTION trial were reported in late 2024, they showed that left atrial appendage closure (LAAC) significantly reduced the risk of nonprocedural bleeding compared with oral anticoagulation (OAC) while maintaining similarly low rates of stroke, death or systemic embolism among patients at moderate to high stroke risk undergoing catheter ablation for atrial fibrillation (AF).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study’s significance got it published in the New England Journal of Medicine, but insights from the trial do not end there. Principal investigator Oussama Wazni, MD, MBA, recently shared other notable lessons learned from OPTION — including data from new secondary analyses — in a late-breaking presentation at the 2025 annual meeting of the Heart Rhythm Society (HRS). These lessons include the following:
“We undertook OPTION to determine how best to approach stroke prevention following ablation for AF,” says Dr. Wazni, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic. “Current guidelines state that the decision whether or not to give anticoagulation after an ablation depends on the patient’s CHA2DS2-VASc score, not on the perceived outcome of the ablation. Yet continuing anticoagulation in higher-risk patients can make them more susceptible to bleeding. So we proposed studying whether closing the LAA, which is where most strokes originate in this population, could protect from stroke and also from bleeding since anticoagulation could be avoided.”
OPTION directly compared LAAC with OAC after AF ablation in 1,600 patients from 114 global sites, all of whom had an elevated CHA2DS2-VASc score (mean of 3.5), indicating moderate to high stroke risk. Patients were randomized 1:1 to undergo LAAC (using the Watchman FLX device) or to continue OAC following ablation. Notably, 95% of patients in the OAC arm received newer nonwarfarin direct oral anticoagulants, predominantly apixaban and rivaroxaban. The trial followed patients for 36 months.
Advertisement
The initial study report yielded the following key findings:
Dr. Wazni’s presentation at the HRS meeting focused on deeper analysis of the OPTION data, yielding the additional insights recapped below.
Advertisement
“The findings from OPTION suggest a paradigm shift in managing stroke risk after AF ablation for eligible patients, as LAAC offers significant bleeding risk reduction relative to OAC while providing comparable stroke protection,” says Mohamed Kanj, MD, Co-Director of Electrophysiology Laboratories at Cleveland Clinic. “Additionally, the ability to avoid chronic OAC therapy is highly appealing to patients, as is the convenience of performing both ablation and LAAC during a single procedure.”
Performing AF ablation and LAAC together is something that Cleveland Clinic has significant experience with, having combined the procedures in more than 500 cases since 2017, primarily in patients who meet the current indication for LAAC — i.e., those at high bleeding risk who need stroke prevention but cannot tolerate OAC therapy. In fact, Dr. Wazni and Cleveland Clinic have led efforts to convince payers that performing these procedures together is clinically appropriate, cost-effective and in patients’ best interest. These efforts helped prompt the Centers for Medicare & Medicaid Services to establish a specific payment code for the combined procedure.
Despite these developments, Dr. Wazni notes that the current indication for LAAC with the Watchman device remains limited to patients who have reason to seek a nonpharmacologic alternative to chronic OAC, such as prior major bleeding or a high risk of bleeding. All patients enrolled in the OPTION trial differed from this indicated population in that they were eligible to take anticoagulation therapy. The OPTION trial sponsor is expected to pursue a new indication for the Watchman device in patients undergoing AF ablation regardless of bleeding risk.
Advertisement
Meanwhile, cost-effectiveness analyses using OPTION trial data are now underway, which will likely inform decisions around broader adoption and reimbursement of LAAC in the setting of AF ablation.
For further perspectives on LAAC and ablation from Drs. Wazni and Kanj, listen to the below episode of Cleveland Clinic's Cardiac Consult podcast for medical professionals.
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2237537/17042806)
The OPTION trial was funded by Boston Scientific, which markets the LAAC device used. Dr. Wazni reports that he has served as a consultant and speaker for Boston Scientific.
Advertisement
Advertisement
OPTION trial demonstrates significantly less bleeding risk with comparable efficacy
Large SURPASS registry study finds LAAO device safe and effective through one year
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Scenarios where experience-based management nuance can matter most
Aim is for use with clinician oversight to make screening safer and more efficient
Multimodal evaluations reveal more anatomic details to inform treatment
A closer look at the impact on procedures and patient outcomes
Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve