Many genetic alterations were related to other malignancies
People with a higher incidence of cancer — multiple melanomas, melanoma and additional cancers or a family history of melanomas and other malignancies — can carry a higher risk for breast, prostate, brain and other cancers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nearly 1 in 5 of 81 patients evaluated, 18.5 percent, had a germline mutation on multiplex genetic testing. In addition, almost half of these mutations were associated with other tumor types.
“These familial traits are not only melanoma. It’s important for patients and their families to know which other cancers they may be at risk for,” says Pauline Funchain, MD, a hematologist and medical oncologist at Cleveland Clinic Cancer Center and lead author of the study.
For clinicians treating familial melanoma, these findings reinforce the importance of sending patients to genetic counseling, says Dr. Funchain, who presented these findings at the 2018 American Society of Clinical Oncology annual meeting in Chicago.
Dr. Funchain and colleagues assessed patients from Cleveland Clinic’s Melanoma Program. In previous research, they found approximately 75 percent of these patients had some family history of cancer.
“Then we drilled down to find out how many have more than three people in their family with cancer — because that’s a lot,” she says. “And that was almost 30 percent.”
In the meantime, a Nordic twin study looking at concordance revealed that melanoma and prostate cancers had the highest heritability.
“We started getting the sense that melanoma is more genetic than not,” Dr. Funchain says. “We knew we were on to something — now we actually had to show it.”
Using patients enrolled in the Gross Family Melanoma Registry, Dr. Funchain and colleagues focused on people with a personal or family history of multiple melanomas and/or other cancer diagnoses.
Advertisement
They tested participants with a multiplex genetic panel for 12 genetic alterations associated with melanoma and 69 associated with other cancers (Invitae Corp., San Francisco). “And lo and behold, not only did we get a decently high rate of people with positive germline mutations… but half of them were found in genes not even believed to be associated with melanoma.”
“There may be a lot about melanoma inheritance that we don’t know because we never really looked,” said Dr. Funchain.
Mutations were observed across melanoma subtypes, including 12 cutaneous, two uveal and one mucosal melanoma. “Uveal melanoma is definitely a different beast than cutaneous melanoma. But we also had a mucosal melanoma that was positive, and that hasn’t been associated with any genes.”
“I think we have enough data to say — regardless of what type of melanoma a patient has — that genetic testing should be considered.”
Going forward, Dr. Funchain would like to tease out the right criteria for which patients to send to genetic counseling, “and then start learning about these genes that have not been associated with melanoma in the past.”
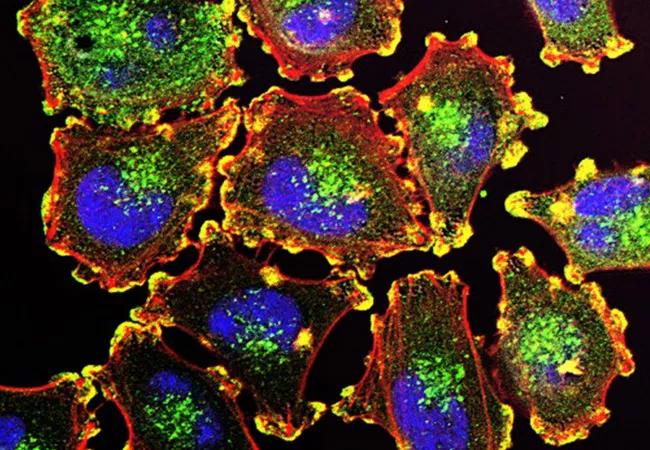
Image: Metastatic melanoma cells. Image source: National Cancer Institute
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors