A multidisciplinary approach facilitates timely diagnosis and better treatment
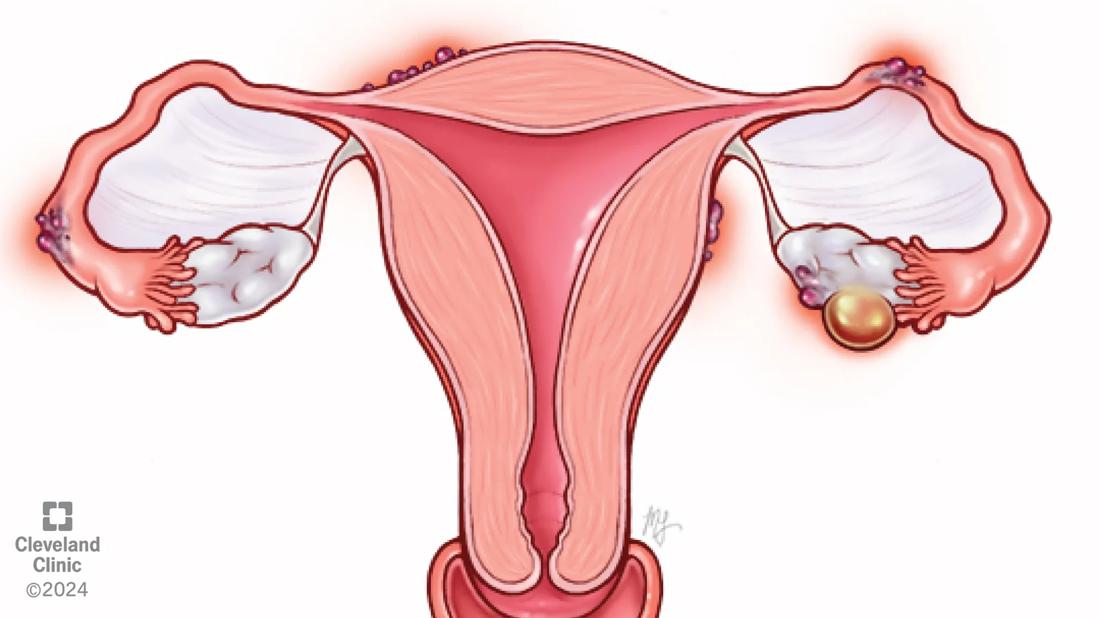
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1b3d06a1-7925-40a7-954b-e78a073de0c8/gut-endometriosis-illustration)
Endometriosis illustration
Endometriosis has a lengthy history of being poorly understood, underdiagnosed and insufficiently treated. While that history is changing, endometriosis can still confound patients and clinicians, in part because its symptoms can mimic or co-occur with gut disorders. Broader awareness among practitioners from many disciplines is key to earlier diagnosis and treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The topic was the focus of a recent review article published in Current Opinion in Obstetrics and Gynecology by Cleveland Clinic specialists in gynecologic surgery, gastroenterology, nutrition and psychology. The researchers concluded that understanding the gut-endometriosis connection is essential for reducing diagnostic delays and delivering optimal patient care.
“When we truly understand the communication between endometriosis and the gastrointestinal systems, we can make more accurate diagnoses and avoid mistakenly labeling endometriosis as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), or vice versa,” says first author Liron Bar-El, MD, a surgical fellow in minimally invasive gynecologic surgery. “This understanding can also inspire innovating research and lead to advancements in diagnosis, monitoring and treatment.”
Greater awareness is needed not only among OB/GYN providers and their patients, but also across other medical specialties, says Cara King, DO, MS, Section Head of Minimally Invasive Gynecologic Surgery and Medical Gynecology at Cleveland Clinic.
“For example, a gastroenterologist may have a patient whose GI symptoms flare during her menstrual period,” says Dr. King. “Without understanding the context of endometriosis, that clinician may miss important indicators of why the patient is suffering. Greater awareness of gut-endometriosis connection can help that GI provider understand the source of the pain and involve an endometriosis specialist in the care of their patient to provide a more comprehensive evaluation and tailored treatment plan.”
Advertisement
Dr. Bar-El adds that awareness is key. Once endometriosis is suspected, the patient should be referred to a specialized endometriosis provider to discuss appropriate treatment, which may include medication, surgery and additional supportive therapies.
“The challenge is actually one step earlier — it’s about getting the patient to the right providers,” she says. “At Cleveland Clinic, our endometriosis specialists are equipped with the knowledge and advanced surgical skills to treat all levels of disease complexity. But if the primary care practitioners, general OB/GYNs and other non-gynecologic specialists don't understand their symptoms and refer them, we won't have the chance to help.”
Among the topics the researchers highlight:
Menstruation-related GI symptoms
Shifting estrogen and progesterone levels affect GI function throughout the menstrual cycle. Bloating, diarrhea, nausea and constipation are more common during menstruation and the luteal phase of the cycle. Overlapping pain pathways and enervation can make digestive pain related to GI contractility seem like gynecologic pain. Endometriosis symptoms, meanwhile, can cause a host of GI symptoms, as well as pelvic pain, menstrual pain, pain with urination, painful bowel movements and pain with intercourse. The researchers found that up to 90% of women with endometriosis experience severe bloating (“endo belly”)or other GI symptoms.
Advertisement
Prostaglandins’ role in endometriosis-related pain
Endometriotic lesions promote production of prostaglandins, leading to hypercontractility, muscle spasms and pain (PGF₂α), and to pain hypersensitization (PGE2). Non-steroidal anti-inflammatory drugs, therefore, can deliver effective relief of discomfort. Research has begun to explore the treatment potential of PGE2 agonists.
Endometriosis and the microbiota-gut-brain axis
Recent research has established links between the gut microbiome and chronic inflammation, affecting hormonal balances and reproductive health. The chronic inflammatory environment can worsen dysbiosis and spur the progression of endometriosis and other gynecologic diseases.
Endometriosis lesions invading the GI tract
Endometriosis lesions in the wall of the bowel can cause fibrosis, leading to narrowing of the intestinal lumen, pencil thin stools and pain with bowel movements. Colorectal endometriosis can mimic malignancies, and appendiceal endometriosis may present with symptoms similar to acute appendicitis. Therefore, endometriosis should always be considered in the differential diagnosis for acute abdominal pain in women of reproductive age.
In addition, the researchers found significant overlap of endometriosis and IBS and IBD. They cited meta-analysis that estimated women with endometriosis were three times more likely to develop IBS than their counterparts without endometriosis. In women with IBS, an estimated 9% to 36% also had endometriosis.
“The takeaway is that effective management of people with endometriosis requires a 360-degree, multidisciplinary approach,” says Dr. Bar-El. “We need to work collaboratively across specialties, using the unique knowledge and expertise of each discipline to deliver well-rounded, comprehensive care.” These specialties may include gastroenterologists, physical therapists, dietitians and pain psychologists.
The Center for Endometriosis and Chronic Pelvic Pain, led by Ashley Gubbels, MD, offers this type of integrated, 360-degree approach to caring for patients with endometriosis and pelvic pain.
Advertisement
“These patients don’t need to suffer! There are multiple evidence-based therapies available,” says Dr. Bar-El. “By collaborating across disciplines, we can build on each other’s foundations to better address their needs, and together we can discover even more ways to help.”
Advertisement
Advertisement
Cara King, DO, MS, outlines practices that can make all the difference
Better screening can improve GI outcomes and reduce costs
Counseling and careful surgical considerations are key
A large nodule had strangulated the patient’s ureter and invaded the vagina, bladder and rectum
Case study: Concomitant robot-assisted surgery without repositioning the patient
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies