Single-center retrospective analysis defies conventional wisdom
Limiting purchases of spinal implants to a single vendor can yield substantial cost savings for a large hospital system without compromising the quality of patient care, suggests a large retrospective cohort study from Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These findings indicate that large hospital systems may do well to consider single-source purchasing as an effective means of reducing healthcare costs while preserving clinical quality,” says Michael Steinmetz, MD, senior author of the study, published in JAMA Network Open (2019;2[11]:e1915567).
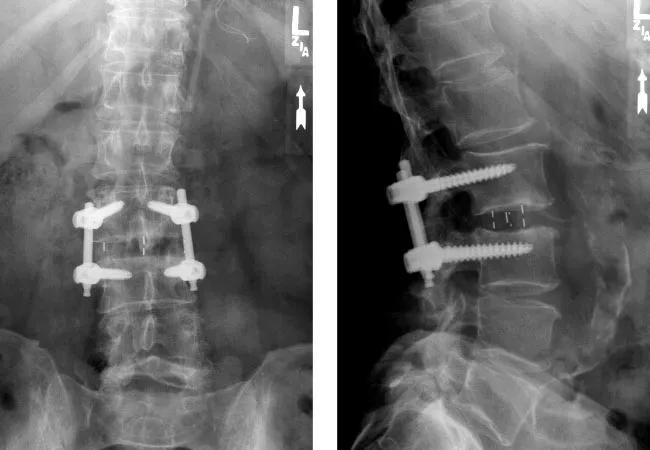
“Spinal fusion surgery is a large and fast-growing category of healthcare spending, and surgical implants represent the largest share of expenditures in this category,” notes Dr. Steinmetz, Chair of Neurosurgery at Cleveland Clinic and a staff surgeon in its Center for Spine Health. “While programs targeting spending on medical devices for cost reduction have been widely reported, particularly in orthopaedics, we’re aware of no studies before ours that assessed cost savings in spine surgery stemming from a single-vendor procurement strategy.”
Over the past decade, Cleveland Clinic adopted a two-component strategy to reduce the cost of its spinal implant purchases:
Advertisement
“Our objective was to realize cost savings on nonspecialized or ‘commodity’ devices while preserving surgeon autonomy in choosing nonstandard or specialty devices,” explains Dr. Steinmetz.
The study was undertaken to quantify resulting cost savings and to assess whether the changes in vendor strategy had any effect on quality of care.
To do so, Dr. Steinmetz and colleagues retrospectively analyzed all adults who underwent single-level lumbar interbody fusion on an inpatient basis at Cleveland Clinic’s Center for Spine Health from January 2009 through July 2017. Patients were categorized according to when their surgery took place:
In addition to annual cost savings under the dual-vendor and single-vendor strategies, the researchers assessed care quality by rates of perioperative complications, revision surgery within 12 months and readmissions within 30 days, as well as by postoperative patient-reported outcomes. The latter were evaluated using the 5-dimension European Quality of Life (EQ-5D) and Patient-Reported Outcomes Measurement Information System-Global Health (PROMIS-GH) instruments.
“We chose lumbar interbody fusion as a proxy for the general quality of care at our high-volume spine center, which performs over 3,500 operations annually, because of the large number and relative homogeneity of these cases,” explains Dr. Steinmetz. Patients with a prior spinal fusion or receiving multilevel or anterior interbody fusion were excluded.
Advertisement
The analysis included 1,373 patients across the 8.5-year study period. Clinical outcomes were as follows after propensity score weighting to adjust for confounders:
Revisions, complications and patient-reported outcomes were statistically equivalent across all three study periods. Readmissions were not statistically equivalent but were also not significantly different, with outcomes favoring the single- and dual-vendor periods over the multivendor period.
Transition from a multivendor to a dual-vendor strategy starting in 2011 was associated with a 24% reduction in annual costs for nonspecialized devices. Simultaneous transition to the initial capitated pricing model for specialty implants was associated with a 35% reduction in annual costs for those products.
In 2015, transition to a single-vendor strategy was associated with a further 21% reduction in annual costs for nonspecialized devices, and refinement of the capitated model was associated with a further 2% decline in annual costs for specialty and MIS devices.
“We found that using a single vendor for nonspecialized, commodity implants was not correlated with any significant differences in perioperative complications, 30-day readmissions, 12-month revision surgeries or patient-reported health status,” says Dr. Steinmetz. “This provides encouraging confirmation that the substantial cost savings we achieved through vendor rationalization did not appear to compromise patient care.”
Advertisement
The authors note that the study is limited by its retrospective design, its focus on one procedure type (albeit a common one) and the short (12-month) duration of its follow-up. They also emphasize that their findings may not be generalizable, particularly to lower-volume centers.
“Nevertheless, these findings defy conventional wisdom that relying on a sole vendor must undercut the financial benefits of price competition among multiple vendors and/or undermine the quality of care,” Dr. Steinmetz concludes. “We look forward to future studies that may confirm these intriguing results.”
Advertisement
Advertisement

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does