Study shows comparable success rates to tongue base dependent epiglottic collapse

A recent retrospective analysis — spearheaded by the Cleveland Clinic — shows that patients with obstructive sleep apnea (OSA) who have independent epiglottic collapse derive the same benefit from hypoglossal nerve stimulator (HGNS) implantation as those with tongue-base dependent epiglottic collapse. These findings, recently presented during the American Academy of Otolaryngology-Head and Neck Surgery Annual Meeting, offer valuable insights that could impact clinical decision-making for this patient population.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
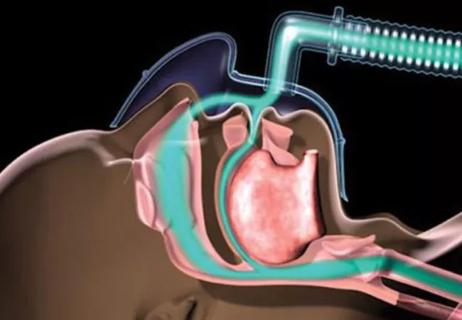
“For patients with obstructive sleep apnea who cannot tolerate continuous positive airway pressure (CPAP), hypoglossal nerve stimulator (HGNS) implantation is a highly effective alternative,” notes study author Alan Kominsky, MD, Otolaryngology and Sleep Medicine, Cleveland Clinic. “Prior to implantation, patients must undergo a drug-induced sleep endoscopy (DISE). This procedure involves sedation and endoscopy to assess the airway, particularly how the palate collapses. The FDA requires the palate to collapse in a flat, rather than a circular, manner for nerve stimulator eligibility.”
During DISE, the entire airway is evaluated, including the lateral walls of the oropharynx, hypopharynx, base of the tongue and epiglottis, he explains. While the hypoglossal nerve stimulator has been shown to work well with tongue-based airway obstructions, its effectiveness for patients with an independent collapse of the epiglottis is less understood and a matter of debate among experts.
“Typical approaches to address independent epiglottic collapse include shortening the epiglottis or denuding the mucosa on the lingual side of the epiglottis and roughening up the lingual tonsil area to encourage adhesion to the base of the tongue so it doesn’t flop independently,” says Dr. Kominsky. “All of these methods are met with varying success and potential complications. We were interested in assessing the success rates of hypoglossal nerve stimulation among these patients.”
Dr. Kominsky and colleagues performed the current study to determine if HGNS implantation was equivalently effective in the management of obstructive sleep apnea in patients with tongue-dependent epiglottic collapse and those with independent epiglottic collapse.
Advertisement
This retrospective chart review included 197 adult patients treated for obstructive sleep apnea with HGNS between November 2015 and July 2023. Patients were assessed based on the following: BMI at the time of HGNS insertion, DISE epiglottic evaluation, sex, BMI, tobacco use, original apnea-hypopnea index (AHI) and efficacy of their implantation in the management of OSA.
For this analysis, researchers defined the efficacy of implantation as a reduction of apnea-hypopnea index from moderate or severe to mild in their first post-operative polysomnogram.
Forty-one patients with tongue base-dependent epiglottic collapse and 27 with independent collapse were identified in this study. Data showed that the overall HGNS insertion success rate of 82.8% for the entire cohort of patients.
When tested individually and adjusted for BMI, sex and smoking status using multivariable regression analysis, there was no significant difference in the success rates of hypoglossal nerve stimulation between patients with tongue base-dependent epiglottic collapse (90.2%) and those with independent collapse (81.5%), Dr. Kominsky and colleagues report. Consistent with other research, the study authors found that each unit increase in BMI was associated with a 16%reduction in the odds of success from implantation.
“Our study demonstrated that the success rates for patients with tongue base dependent epiglottic collapse versus those with independent epiglottic collapse were very similar,” notes Dr. Kominsky, while emphasizing the significance of this finding. “As a field, there has been no strong consensus on how to handle epiglottic collapse. Surgeons often share personal experiences; however, there is no definitive approach due to the lack of data.
Advertisement
“This research suggests that the epiglottis does not need to be addressed prior to hypoglossal nerve stimulator implantation, potentially saving patients from an unnecessary surgery,” he continues. “While, in most cases, surgical intervention has no immediate effect on swallowing, there are concerns that issues may arise later in life. Avoiding epiglottic surgery could reduce the potential long-term risk of dysphagia as patients age.”
The work of Dr. Kominsky and colleagues paves the way for a new approach to manage patients with obstructive sleep apnea who have independent epiglottic collapse. “To my knowledge, this hasn’t been looked at before,” he notes. “It is my hope that this research adds a new avenue of thought for clinicians who are contemplating how to treat obstructive sleep apnea patients with independent epiglottic collapse on sleep endoscopy.
“I believe that this opens the door to a data-driven discussion on a patient population where previous conversations have led to no definitive answers,” he adds. The next step, according to Dr. Kominsky, involves further research. “There is power in numbers. We need additional studies or a multi-institutional review of outcomes to gather a larger patient base to strengthen our conclusions.”
When asked how these findings will affect how care is provided at Cleveland Clinic, Dr. Kominsky shares his confidence in the approach. “When I counsel patients following their drug-induced sleep endoscopy, which shows an independent epiglottic collapse, rather than have the discussion about trimming the epiglottis, I will be able to discuss their options, including that the hypoglossal nerve stimulator has a positive track record of improving the airway without having to directly operate on the epiglottis.”
Advertisement
Advertisement
Device features, desensitization strategies can help

Screening tool helps flag conditions that warrant further attention

Patients with epilepsy should be screened for sleep issues

A deep dive into the evolution of surgical sleep therapy

Cleveland Clinic study finds that durable weight loss is key to health benefits

Novel procedures provide options for patients who can’t tolerate CPAP

Large cohort study suggests need for routine sleep screening as part of neurological care

A review of conservative, pressure-based and surgical treatments for OSA