BTK inhibitor tolebrutinib shows positive results in phase 3 HERCULES trial
The first clinical trial evidence has been published showing that a therapy can delay confirmed disability progression in patients with nonrelapsing secondary progressive multiple sclerosis (MS).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The unprecedented finding is from HERCULES, a phase 3 trial of the investigational oral BTK inhibitor tolebrutinib that demonstrated a 31% delay in the onset of six-month confirmed disability progression — the primary endpoint — compared with placebo. The results were just published in full in the New England Journal of Medicine and presented at the American Academy of Neurology's 2025 annual meeting by Robert Fox, MD, chair of the study’s global steering committee. Dr. Fox presented initial results at the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) meeting last September.
“This result reflects clear progress toward an effective therapy for delaying disability progression in patients with secondary progressive MS, a population for which there are no therapies with demonstrated efficacy,” says Dr. Fox, first author of the study and a neurologist in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research.
“Current disease-modifying therapies for MS have limited effects on the accrual of disability, particularly on disability progression that’s independent of relapses, which is believed to be due in large part to chronic neuroinflammation in the CNS involving myeloid cells such as microglia,” Dr. Fox notes.
Tolebrutinib is a brain-penetrant member of a new class of oral drugs known as Bruton tyrosine kinase (BTK) inhibitors that are FDA-approved for treatment of lymphomas and lymphoid blood disorders. The drug is thought to work by modulating B lymphocytes and activated microglia in the central nervous system (CNS), with possible activity on the peripheral immune system as well. “These actions explain the interest in tolebrutinib for nonrelapsing secondary progressive MS,” Dr. Fox says, “as the drug appears to address some of the underlying mechanisms of disability accumulation associated with neuroinflammation in the brain and spinal cord.”
Advertisement
The phase 3 HERCULES trial focused on individuals with nonrelapsing secondary progressive MS, who experience a gradual but relentless worsening of function and increase in disability over time. A total of 1,131 patients aged 18-60 years were randomized from multiple centers worldwide, including Cleveland Clinic. All patients had documented disability progression in the 12 months prior to screening but no clinical relapses in the 24 months before screening, with an Expanded Disability Status Scale (EDSS) score from 3.0 to 6.5 at screening.
“The aim was to test the hypothesis that tolebrutinib could influence progression independent of relapse activity,” Dr. Fox explains. “These individuals with nonrelapsing secondary progressive MS have been the group of patients for whom it’s been hardest to find therapies because they don’t have peripherally driven inflammation.”
Participants were randomized 2:1 to receive oral tolebrutinib 60 mg daily (n = 754) or placebo (n = 377) in a double-blind manner. Treatment lasted 24 to 48 months, with all patients continuing until a prespecified number of six-month confirmed disability progression (CDP) events occurred. The primary endpoint was the time to onset of six-month CDP, defined as an increase from baseline EDSS score of ≥ 1.0 point (for baseline scores ≤ 5.0) or ≥ 0.5 points (for baseline scores > 5.0) confirmed over at least six months.
Over median follow-up of 133 weeks (interquartile range, 108-157 weeks), the cumulative incidence of six-month CDP was 22.6% in the tolebrutinib group versus 30.7% in the placebo group (hazard ratio [HR] = 0.69; 95% CI, 0.55-0.88; P = .003).
Advertisement
A similar degree of risk reduction with tolebrutinb was observed in the time to three-month CDP (HR = 0.76; 95% CI, 0.64-0.92; P = .01). Additionally, a significantly higher proportion of patients achieved improvement in disability with tolebrutinib therapy, with a six-month confirmed disability improvement rate of 8.6% versus 4.5% with placebo (HR = 1.88; 95% CI, 1.10-3.21). Measures of a three-month sustained 20% increase in the timed 25-foot walk test favored tolebrutinib, but tolebrutinib had no impact on the proportion of patients with a 20% increase in 9-hole peg test time.
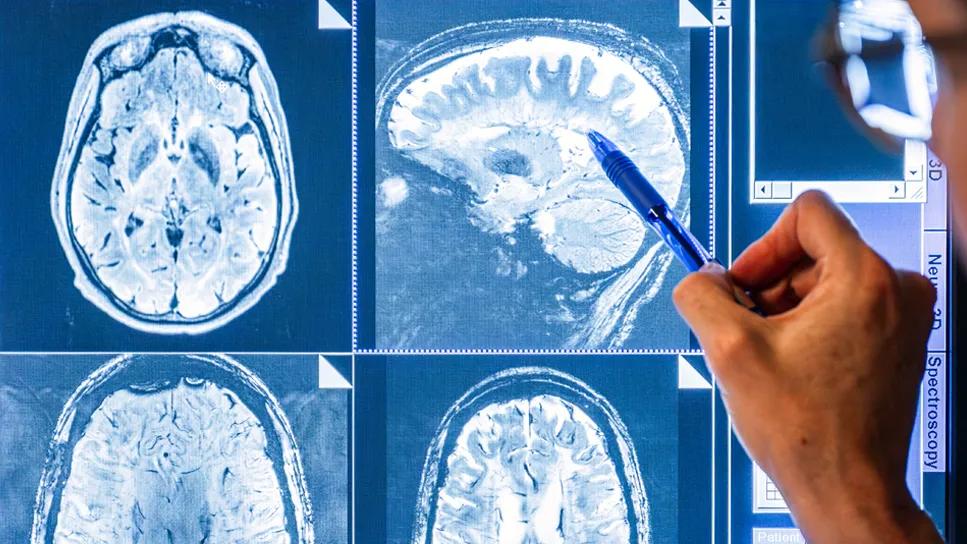
The mean annualized rate of new and/or enlarging T2-weighted lesions on brain MRI was reduced significantly with tolebrutinib compared with placebo (1.84 vs. 2.95; P = .01). “This is consistent with tolebrutinib’s effect on the peripheral immune system, specifically B lymphocytes,” Dr. Fox notes. There was no significant difference in whole brain volume loss between the groups. “This is surprising,” he says, “given that whole brain volume had up to now been considered a useful treatment-response biomarker for progressive MS.”
Adverse event rates were broadly comparable between the tolebrutinib and placebo groups, although serious adverse events were more frequent with tolebrutinib. However, alanine aminotransferase (ALT) levels above three times the upper limit of normal (ULN) were observed in 4.0% of tolebrutinib recipients versus 1.6% of placebo recipients over the course of the trial. ALT level increases above 20 times ULN were reported in 0.5% of tolebrutinib recipients versus 0% of placebo recipients.
Advertisement
Notably, all cases of severe ALT elevation (>20 times ULN) occurred within 90 days of treatment initiation. This prompted implementation, partway through the trial, of more frequent (weekly) liver monitoring during the first three months of treatment to allow early detection of ALT increases. Prior to protocol implementation, one tolebrutinib recipient with severely elevated ALT died of complications related to liver failure. After adoption of weekly monitoring, all instances of elevated liver function enzymes resolved without sequelae.
“HERCULES is the first positive trial of a therapy for use in nonrelapsing secondary progressive MS,” Dr Fox says. Tolebrutinib is currently under review by the U.S. Food and Drug Administration (FDA).
If the drug is cleared for use in MS, approval will likely require intensive monitoring of liver function enzymes during the first three months of therapy, Dr. Fox says, with less-frequent monitoring thereafter. “It appears that about one in 200 patients will have severe elevation of liver enzymes during the first three months of use,” he notes, “so careful monitoring is important and the drug should be stopped immediately in those with liver enzyme elevations.”
He adds that this risk of liver dysfunction is likely to be a class effect for BTK inhibitors, several of which are also in clinical development for treatment of MS and have been issued clinical holds by the U.S. FDA. Additionally, tolebrutinib is being evaluated for treatment of primary progressive MS in the ongoing phase 3 PERSEUS trial (NCT04458051). Results of that study, in which Cleveland Clinic is also participating, are expected by the end of the year.
Advertisement
HERCULES was sponsored by Sanofi, the developer of tolebrutinib. Dr. Fox reports consulting for, and receiving research support from, Sanofi and other pharmaceutical companies.
Advertisement

Mixed results from phase 2 CALLIPER trial of novel dual-action compound

A co-author of the new recommendations shares the updates you need to know

Rebound risk is shaped by patient characteristics and mechanism of action of current DMT

First-of-kind prediction model demonstrates high consistency across internal and external validation

Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

This MRI marker of inflammation can help differentiate MS from mimics early in the disease

Focuses include real-world research, expanding access and more