New report highlights experience, early outcomes

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/783a3a15-9f08-4848-bd57-652bfb595755/650x450-Kaouk_jpg)
650×450-Kaouk
A team of urologists at Cleveland Clinic is the first to report their experience and the early outcomes of a transvesical radical prostatectomy and pelvic lymph node dissection using the single-port (SP) robot system. They published their insights in Urology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The team has completed more than 50 cases to date, explains Jihad Kaouk, MD, Director of the Center for Robotic and Image-Guided Surgery at the Glickman Urological & Kidney Institute, surpassing the number reported in the journal. So far, the team is heartened by the results they’ve seen.
The authors conclude that for select low-risk prostate cancer patients, this approach demonstrates intraoperative safety and good postoperative recovery.
Robot-assisted radical prostatectomy (RARP) has edged out open radical prostatectomy (RP) in recent years as a preferred treatment for localized prostate cancer. Still, there are opportunities for improvement in robot-assisted techniques, says Dr. Kaouk, who is also Institute Vice Chair for Surgical Innovations and holds the Zegarac-Pollock Endowed Chair in Laparoscopic and Robotic Surgery.
And that’s where the SP system can make an impact, he says. The single-arm allows 360-degree multi-quadrant access. This design enables the robot to operate in a smaller anatomical space, resulting in decreased postoperative pain.
Of note, multiport RARP used to require five incisions in a patient’s abdomen, but at Cleveland Clinic with SP extraperitoneal RARP, it requires only one. It used to require a one- to two-night hospital stay; now, it’s generally an outpatient procedure. Most patients follow a postoperative non-narcotic pain regimen.
The SP extraperitoneal RARP approach also allows the patient to lie flat on the table, without the need to be in a steep Trendelenburg position, which can initiate perioperative complications, such as optical nerve edema, congestion and respiratory problems.
Advertisement
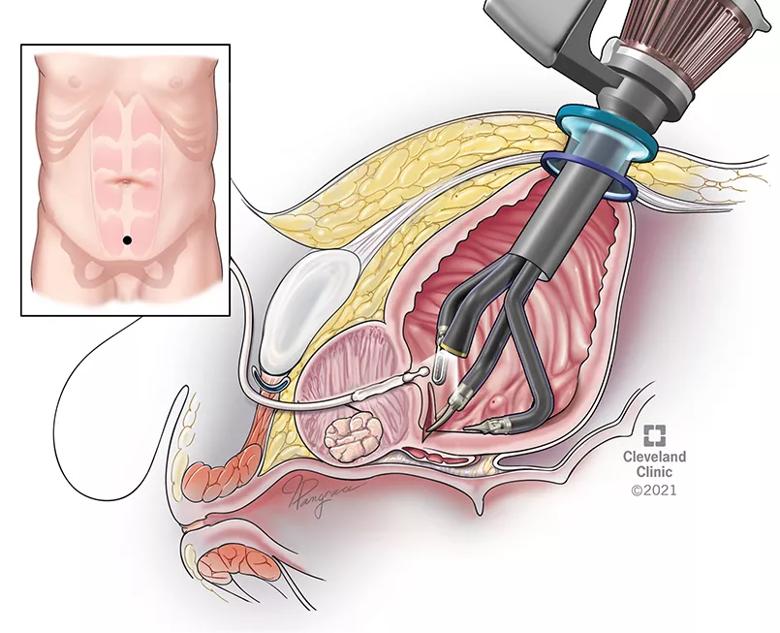
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e4b3265e-4adb-4b66-b088-3f86fb604f48/21-URL-2188442-Inset-1_jpg)
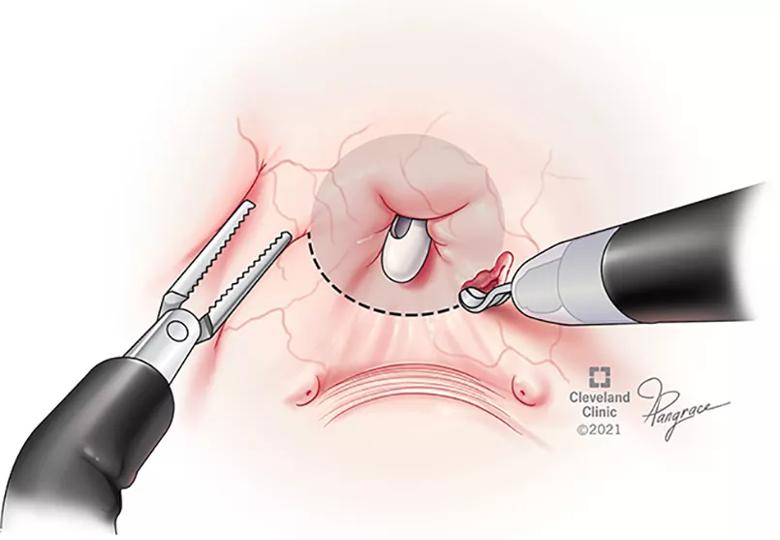
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0eb646b7-7634-40a1-99b5-20a5f17edf06/21-URL-2188442-Inset-2_jpg)
View of the bladder trigone from inside the bladder from the robot camera
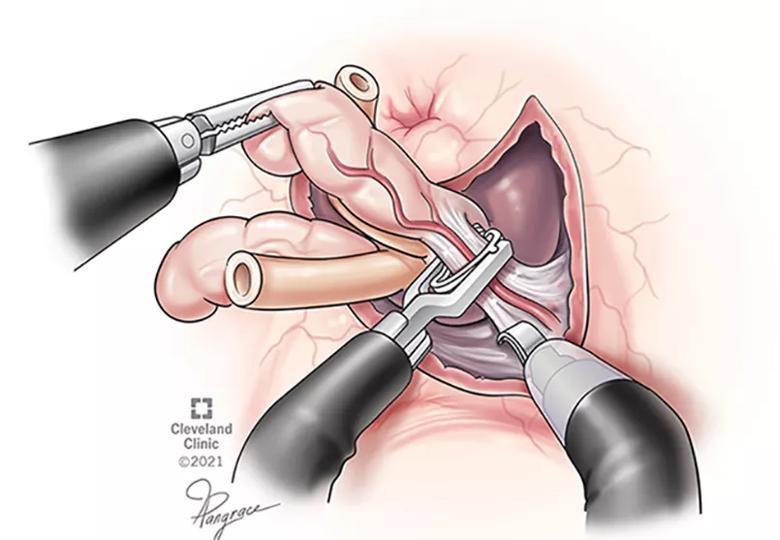
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e31e3658-32ef-488c-881a-7298d8a4c396/21-URL-2188442-Inset-3_jpg)
Right seminal vesicle dissection and clipping using robotic weck clip applier.
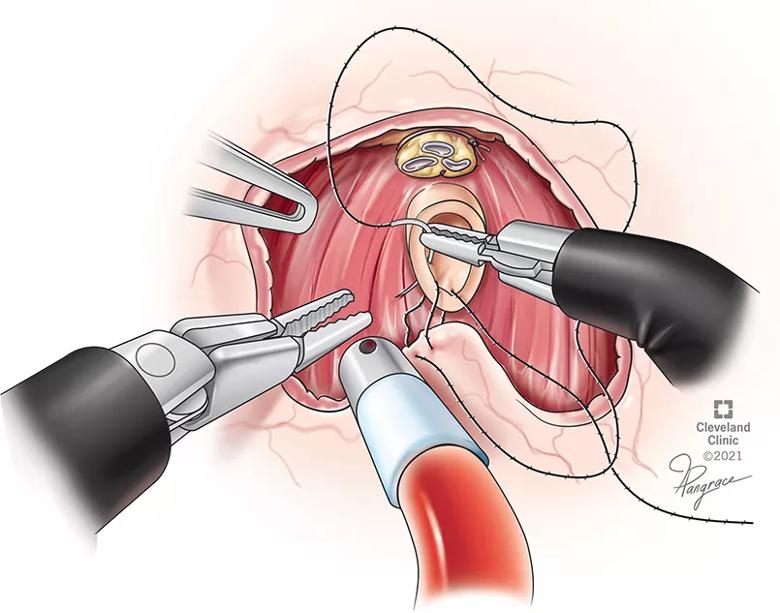
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3de27e01-7800-492c-8e89-59388cc0dba2/21-URL-2188442-Inset-5_jpg)
Vesicourethral anastomosis using 3-0 V-lock on an RB-1 needle. In this case, two sutures are needed measuring 9 and 6 in, respectively.
The transvesical RARP approach, Dr. Kaouk says, shares all of these benefits; however, patients are experiencing better postoperative urine control.
“Incontinence is a big issue for patients undergoing prostatectomy,” he says. “We are seeing a significant advancement in this approach that, honestly, has exceeded our expectations.”
In the Urology study, 95% of patients achieved continence within two to seven days following the removal of the Foley catheter. The anatomical entry point – a 3cm suprapubic incision into the bladder – prevents unnecessary dissection of the bladder and bowel mobilization. It also helps prevent lysis of adhesions and potential intestinal damage.
Dr. Kaouk says that implementing an SP transvesical RARP procedure was a natural extension of the team’s experience using the same approach but for a simple prostatectomy, as well as the SP extraperitoneal RARP. These experiences were instrumental in the development of this technique, he says.
On its initial use, he says it was used to avoid entry into the intraperitoneal space for patients with previous abdominal surgeries, but given its successful outcomes, the team will add the technique to its ever-growing trove of innovative robotic approaches.
Advertisement
Even though more studies are needed, Dr. Kaouk says the team is enthused by their experience so far with this approach, concluding, “We know it’s a good therapeutic option for cancer control and offers what may be better quality of life outcomes for our patients.”
Reference
Kaouk J, Beksac AT, Zeinab MA, Duncan A , Schwen ZR, Eltemamy M. Single Port Transvesical Robotic Radical Prostatectomy: Initial Clinical Experience and Description of Technique, Urology (2021), doi: https://doi.org/10.1016/j.urology.2021.05.022
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key