First-of-kind study is testing feasibility of real-world practice model

Cleveland Clinic’s Center for Neurological Restoration is conducting a first-of-its-kind clinical trial investigating the feasibility and fidelity of in-home teleneuropsychological testing for patients with Parkinson’s disease (PD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During the trial, participants with PD will be randomized to standardized neuropsychological testing and procedures delivered face-to-face or through a HIPAA-compliant videoconferencing platform. To date, no published studies have systematically evaluated this type of unassisted, in-home approach in this clinical population.
“Neuropsychological testing is the gold standard for assessing cognition and memory,” says principal investigator Scott Sperling, PsyD, ABPP-CN. “Since the COVID-19 pandemic, a growing number of studies have been published regarding its use in a virtual setting. The vast majority of these studies, unlike ours, have significant limitations, such as requiring involvement of a caregiver or that patients go to a telemedicine studio.”
The potential benefits of teleneuropsychology are particularly high for patients with PD, who have highly complex motor, cognitive and behavioral symptoms that can cause substantial burden and require a range of specialized healthcare services. Use of the technology, the investigators believe, could help meet the needs of individuals in areas with less access to care and reduce the indirect costs incurred by patients and caregivers for travel to in-person evaluations.
“For patients with Parkinson’s, there is no shortage of barriers to getting high-quality evaluations,” Dr. Sperling says. “These include the safety risks inherent in coming to the clinic because of balance issues. Our ultimate goal is to validate the in-home teleneuropsychology practice model to support its broad implementation" to improve patient outcomes.
Advertisement
Epidemiologic data indicate that 50% of patients develop dementia within 10 years of a PD diagnosis, making neuropsychological testing critical for this population. Only 3% to 15% of neuropsychologists use telemedicine to conduct the testing, according to available studies.
Funded with a $100,000 grant from Cleveland Clinic’s Healthcare Delivery and Implementation Science Center, the study aims to enroll 160 patients with mild to moderate PD and common comorbidities who are representative of the broader population with PD. Participants also must have access to a stable internet connection and a desktop computer, laptop or tablet with a web camera.
Participants are randomized 1:1 to either face-to-face neuropsychological evaluation or evaluation via in-home teleneuropsychology. After randomization, all patients undergo evaluation at baseline and again either four weeks later (n = 60) or one year later (n = 100). The two different time frames are used in order to assess both short-term and long-term test-retest reliability. Within the subgroup retested at four weeks, patients are again randomized to either face-to-face or virtual evaluation, introducing a crossover aspect to further assess test consistency.
The evaluation of fidelity includes establishing the reliability of teleneuropsychological testing, its diagnostic validity, and one-year change in cognitive scores among participants. The neuropsychological tests, which are well validated and commonly used in clinical practice, will be administered by two trained research assistants in both the face-to-face and virtual study arms. Standardized testing instructions and procedures will be used in both settings, with modest modifications in the virtual setting (e.g., instructions for the participant to look at the stimulus on the computer screen rather than on the desk in front of them).
Advertisement
“Most prior telehealth validation studies have been limited to the evaluation of telephone-based cognitive screening instruments,” Dr. Sperling notes. “This study will efficiently and effectively address multiple critical research questions about teleneuropsychological testing that have direct and significant clinical implications for patient outcomes.”
Besides rigorously evaluating the technology, the investigators also will administer questionnaires to patients at baseline, four weeks and one year in both study arms to assess patient satisfaction. “We will be systematically collecting specific information related to any difficulties experienced during the evaluations, such as disrupted connections,” Dr. Sperling says. “The data will allow us to refine the practice model and make best-practice recommendations before full-scale implementation.”
The researchers’ primary hypothesis is that there will be moderate to high correlations between individual neuropsychological test scores obtained during the in-home tele-neuropsychology evaluations and the face-to-face sessions. The hope is that the study will support implementation of a teleneuropsychology practice model for patients with PD at Cleveland Clinic and foster broad implementation and maintenance in healthcare settings across the United States.
“If our study validates this model,” Dr. Sperling says, “there is no reason why we can’t replicate the research across other neurodegenerative and neurological diseases, such as Alzheimer’s disease, Lewy body dementia or multiple sclerosis.”
Advertisement
Advertisement

Various AR approaches affect symptom frequency and duration differently

Dopamine agonist performs in patients with early stage and advanced disease

Early assessment could affect clinical decision making

Systems genetics approach sets stage for lab testing of simvastatin and other candidate drugs

Study aims to inform an enhanced approach to exercise as medicine

New tool for general neurologists aims to streamline differential diagnosis

When and how a multidisciplinary palliative care clinic can fill unmet needs for this population
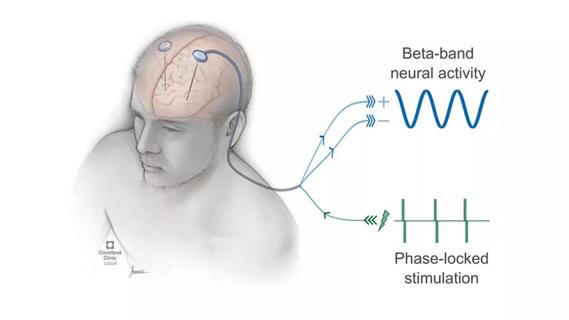
Research project will leverage insights into neural circuits to advance DBS technology