Retrospective reports fuel cautious optimism for broader use

Options for treating intracranial aneurysms expanded with the introduction in 2011 of flow diversion stenting, in which blood flow is selectively diverted away from the weakened artery wall to prevent rupture and promote vessel healing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Approved by the FDA to treat aneurysms ≥ 1 cm in the anterior circulation, flow diverter therapy is now drawing interest for smaller, atypical and posterior-circulation aneurysms — all of which are poor candidates for conventional treatments. In a series of three retrospective analyses published late last year, Cleveland Clinic became one of the first U.S. centers to report results from these emerging applications.
“It’s important to note that our studies were not prospective randomized trials, but they nevertheless provide quite useful information,” says Gabor Toth, MD, a vascular and interventional neurologist with Cleveland Clinic’s Cerebrovascular Center and corresponding author of the studies. “Flow diversion appears to work relatively safely for many different types of aneurysms as long as patients and aneurysms are selected carefully, with an understanding of the technology and its limitations, and as long as procedures are done at experienced centers by experienced operators.”
He notes that the primary goal of flow diverter therapy is to redirect blood flow away from the aneurysm toward the normal flow route and provide a scaffolding for later neo-endothelial proliferation and vessel wall healing. While diverter stents resemble conventional stents, they have higher surface metal coverage and lower porosity to facilitate aneurysm occlusion.
The largest of the recent Cleveland Clinic analyses focused on tandem intracranial aneurysms — i.e., two or more aneurysms in close proximity on the parent vessel with no identified systemic disease associated with their appearance. Stent-assisted coiling for wide-necked aneurysms has been the traditional endovascular strategy for these aneurysms, but the need for multiple catheterizations or interventions complicates treatment.
Advertisement
Dr. Toth and colleagues reviewed 20 patients (all women) with tandem intracranial aneurysms treated at Cleveland Clinic between 2011 and 2016 (World Neurosurg. 2017;107:142-147). The patients collectively had 47 tandem intracranial aneurysms, all of which were successfully treated in one session.
Among patients with available follow-up imaging, 85 percent of 40 aneurysms showed complete occlusion, and all patients had a favorable clinical outcome.
Three patients (15 percent) experienced mild transient symptoms, including quickly resolving speech issues in two patients and transient arm weakness in one.
The authors concluded that flow diverter therapy appears to be technically feasible, safe and effective for tandem intracranial aneurysms, although larger prospective studies were needed for confirmation.
Blood-blister-like aneurysms (BBAs) are small, fragile bulges occurring in nonbranching vessels (see image below). Subarachnoid hemorrhage is the most common manifestation of these aneurysms, which account for around 1 percent of all intracranial aneurysms.
Because of their small size, BBAs are often not identified until days after a bleed. They likewise are challenging to treat, with high re-rupture rates.
In a retrospective review involving eight patients with ruptured BBAs (Neuroradiology. 2017;59:1285-1290), Dr. Toth and colleagues found that flow diversion was associated with no re-ruptures, retreatments or aneurysm recurrences. Most patients were treated two days or more after the initial bleed.
Advertisement
All eight patients received dual antiplatelet therapy, and good clinical outcomes (Rankin score 0-2) were reported in six of seven patients (85.7 percent) with available follow-up at one year.
Complete occlusion of the aneurysm on angiogram or MRI was seen in six of the eight patients at a median follow-up of eight months.
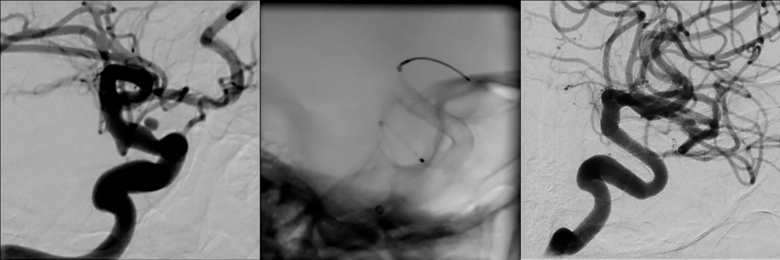
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/669a436a-5f78-4a26-9bd6-7f7d78de0cec/18-NEU-734-Flow-diverter-Inset_png)
Series of images showing a blood blister-like aneurysm before treatment (left), with a flow diverter device deployed in the artery (middle) and after flow diverter treatment, where the aneurysm is now healed (right).
Intracranial vertebral artery dissecting pseudoaneurysms are a rare, but increasingly recognized, cause of subarachnoid hemorrhage and stroke. The risk for re-rupture is high.
Dr. Toth and colleagues reported on eight vertebral artery dissecting pseudoaneurysms in seven patients treated with flow diverter stents, including four patients with ruptured aneurysms (J Neurointerv Surg. 2017;9:1014-1018). Seven of the eight aneurysms were treated with a single flow diverter device, and three were concurrently coiled.
Complete occlusion was achieved in six of eight aneurysms at a median follow-up of 14 months. Two patients had periprocedural strokes with transient neurologic deficits. Both had full recoveries with no residual neurologic deficits.
Dr. Toth says the Cleveland Clinic experience suggests that flow diverter therapy for atypical intracranial aneurysms “carries great promise but has limitations, and is not the ultimate answer to all aneurysms.”
Advertisement
He concludes: “Operators should carefully consider the risks and benefits of all treatment options before proceeding with this therapy.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help