Findings may lead to new treatments to delay Alzheimer onset
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In recent years, prevention has become a major focus of Alzheimer disease (AD) research because once AD pathology has advanced, treating patients at this stage does little to slow disease progression or improve cognitive function.
The focus of our research at Cleveland Clinic and increasing numbers of other centers has therefore been identifying the brain changes that happen a decade or more before clinical symptoms manifest and finding biomarkers that can be used to assess interventions that can slow or prevent disease progression.
If we can delay onset of the disease by five years, we can reduce the number of people with AD by about 50 percent. If we delay onset by 10 years, we can reduce the number by 85 percent and virtually eliminate this enormous health problem.
We have recently made significant progress in achieving these goals. Research has shown that the brain compensates for age-related neural deficits by working harder to maintain cognitive functioning; this brain activation is greater in people at genetic risk for AD than in those at lower risk, which may represent an early response to AD pathology.
Investigators from Cleveland Clinic’s Schey Center for Cognitive Neuroimaging recently helped lead a multicenter collaboration to conduct the first longitudinal study to find out how this activation evolves over time and whether it persists or declines with the onset of cognitive impairment. Our full results were published earlier this year in Neuroimage.
For five years, we tracked brain activity in 45 participants ages 65 to 85 who were cognitively intact at study onset. We categorized these participants as follows:
Advertisement
Participants were evaluated at baseline, 18 months and 57 months. They underwent functional MRI (fMRI) screening, neuropsychological testing and a test we developed and evaluated in past studies: task-activated fMRI.
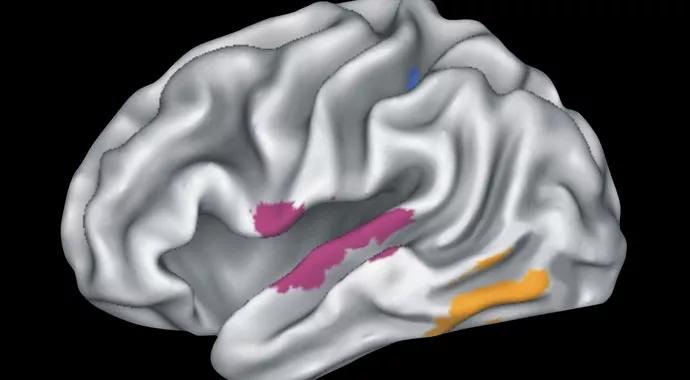
In this task-activated fMRI, participants perform a memory task that involves recognizing the names of famous people while fMRI records their brain activity. We have found task-activated fMRI to be very effective at activating the semantic memory network of the brain ― hippocampus, posterior cingulate, anterior cingulate and temporoparietal regions ― that is vulnerable to the earliest pathological changes in AD.
At baseline, the high-risk group had greater brain activation in the semantic memory network than did the low-risk group. Over the course of the study, however, brain activation decreased in the high-risk group while it progressively increased in the low-risk group. These results demonstrate how the compensatory response diminishes with increased AD-related pathology but continues to function in response to the normal neural damage associated with aging.
These findings have significant implications: They have validated task-activated fMRI as a biomarker that is sensitive to the changes in the brain during the preclinical phase of AD. We can use this biomarker to evaluate interventions ― such as physical activity and medications ― to determine whether they maintain brain activation in people at high risk. If brain activation can remain high, at-risk individuals can maintain their cognitive performance for a longer period of time.
Advertisement
We currently have a clinical trial in progress that is using task-activated fMRI to evaluate donepezil HCl (Aricept), which is commonly prescribed for people diagnosed with mild to moderate AD, for use in people with a genetic risk of AD who still have normal cognitive function. We are also applying for a grant to use task-activated fMRI to evaluate physical activity and brain activation, and we plan to continue research to better understand brain activation and AD.
Dr. Rao holds the Ralph and Luci Schey Endowed Chair and is Director of the Schey Center for Cognitive Neuroimaging in Cleveland Clinic’s Lou Ruvo Center for Brain Health.
Advertisement
Advertisement

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does