Prevalence, characteristics and disease course
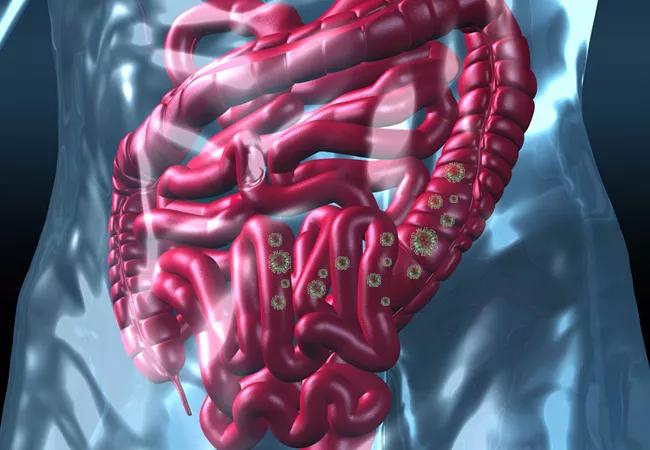
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ca2160c7-f669-430a-a9b0-c36cc15bf02a/21-DDI-2066394-CCJM-Curbside-GI-Manifestations_jpg)
21-DDI-2066394-CCJM-Curbside-GI-Manifestations
Healthcare providers should be aware of the GI manifestations of COVID-19 and perform SARS-CoV-2 testing in patients presenting with digestive changes, especially those with respiratory symptoms, according to a recent review article published in Cleveland Clinic Journal of Medicine’s COVID-19 Curbside Consult series. In this article, Cleveland Clinic’s Sara El Ouali, MD, Jean-Paul Achkar, MD, Bret Lashner, MD, and Miguel Regueiro, MD, discuss gastrointestinal manifestations of COVID-19.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Studies have found SARS-CoV-2 RNA in the stool; in esophageal, gastric, duodenal and rectal biopsies, and in GI and liver tissue. Although the pathophysiology of digestive symptoms in COVID-19 remains unclear, data have shown that SARS-CoV-2 appears to enter host cells via the angiotensin-converting enzyme-2 (ACE2) receptor, which is highly expressed in the small bowel and colon. Other studies show viral infection of enterocytes in small intestinal organoids.
Originally, data from Wuhan in early 2020 indicated that the prevalence of GI symptoms in patients with COVID-19 was fairly low, at 2%-10%. However, larger, subsequent studies reported higher rates, at 16.1% in China and 33.4% in other countries.
The most commonly reported GI symptoms associated with COVID-19 are loss of appetite, diarrhea, nausea or vomiting, and abdominal pain.
There is contradicting data about whether or not GI symptoms in COVID-19 are associated with a worse disease course and prognosis. Among the largest studies is a retrospective study of 29,393 patients with COVID-19, GI symptoms were associated with a 50% increased risk of severe illness. This same study found that patients presenting with GI symptoms and fever had an increased risk of severe COVID-19.
According to the authors, management of COVID-19-associated GI symptoms is mainly supportive and individualized according to the patient’s symptoms, including: fluid and soup intake, and oral or intravenous rehydration. Pharmacotherapy may include prochlorperazine or ondansetron for nausea and vomiting, and loperamide for diarrhea.
Advertisement
Advertisement
Patients report improved sense of smell and taste
Clinicians who are accustomed to uncertainty can do well by patients
Unique skin changes can occur after infection or vaccine
Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition
As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients
Early results suggest positive outcomes from COVID-19 PrEP treatment
Could the virus have caused the condition or triggered previously undiagnosed disease?
Five categories of cutaneous abnormalities are associated with COVID-19