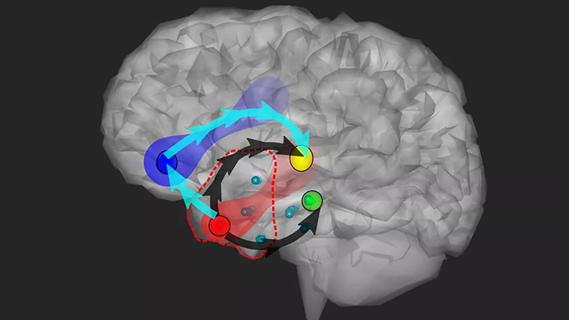
Data-driven methods may improve seizure localization and refine surgical decision-making
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/14186230)
Approximately one-third of people with epilepsy have seizures refractory to medications. For those patients, surgery offers the best chance for decreased seizure burden and perhaps seizure freedom. However, no more than 1% to 2% of North American patients who would benefit from surgery are referred to a surgeon’s office.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Demitre Serletis, MD, PhD, an associate professor and neurosurgeon in Cleveland Clinic’s Epilepsy Center, is working to create a data-driven process — merging concepts from neuroengineering, artificial intelligence (AI) and machine learning — to improve care and outcomes for these types of patients.
“This is the era of brain exploration,” says Dr. Serletis, who is also a researcher with the Department of Biomedical Engineering in Cleveland Clinic Lerner Research Institute. “We open the skull, we resect some of the brain tissue there and we sometimes place devices — all in a very coordinated, methodical way. We must now curate and learn from this experience. That will allow us to shape future directions in an informed fashion.”
In the latest episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Serletis discusses his research and the future of epilepsy surgery and treatment. He covers:
Click the podcast player above to listen to the 30-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
Advertisement
This activity has been approved for AMA PRA Category 1 Credit™ and ANCC contact hours. After listening to the podcast, you can claim your credit here.
Dr. Serletis: We’d like to learn a bit more about the dynamical principles that lead to seizure start and spread. Can we predict it? As surgeons, we put 15 or 20 electrodes in the brain. There is risk with every single pass, and we’re never sure that we’re going to be right in the exact spot. So, can we extrapolate to better refine the analysis?
Ultimately, this will allow us to build a dynamical platform where we are no longer reviewing just clinical data but also the mathematical and dynamical aspects of this, to enable characterization of patients into profiles that allow us to predict who will benefit from what therapy. At the same time, this will also provide a better way to inform industry on how to design devices to best stimulate the brain.
Advertisement
Advertisement

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Patients with epilepsy should be screened for sleep issues

Sustained remission of seizures and neurocognitive dysfunction subsequently maintained with cannabidiol monotherapy

Model relies on analysis of peri-ictal scalp EEG data, promising wide applicability

Investigational gene approaches offer hope for a therapeutically challenging condition
Study combines intracranial electrophysiology and SPECT to elucidate the role of hypoperfusion

Characterizing genetic architecture of clinical subtypes may accelerate targeted therapy

Pre-retirement reflections from a pioneering clinician, researcher and educator