Reforms aim to address escalating healthcare spending with new global care-delivery strategies
Escalating global healthcare expenditures coupled with aging populations and the commensurate rise in chronic diseases are compelling medical providers and policymakers to shift their focus from traditional fee-for-service models to value-based care programs. Although such reforms aim to improve the value of patient care, with the best possible outcomes per dollar spent, healthcare leaders face substantial challenges when putting value-based models into practice.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A commentary in the June issue of NEJM Catalyst Innovations in Care Delivery addresses these obstacles by describing Cleveland Clinic’s experience developing, operating and refining value-based care models in the United States and United Arab Emirates (UAE). Current literature offers examples of promising care delivery models, but evidence is lacking on how to design, implement and sustain payer-provider partnerships in international markets, including infrastructure investments, operational changes and contractual best practices, explains Joshua Snowden-Bahr, JD, MHA, Regional Director of Contracting and Business Development (International Markets) at Cleveland Clinic.
“Because the public sector is now assuming a greater proportion of costs, healthcare leaders are seeking to develop financing arrangements and care-delivery strategies aimed at reducing the financial burden and improving population health,” he says. “Although data is still emerging, we are beginning to develop blueprints for resolving some of the most pressing issues, ranging from misaligned incentives resulting from fee-for-service payment structures, to infrastructure gaps, to burdensome regulations.”
As Cleveland Clinic has evolved from predominately a provider of surgical, complex specialty care to a more population health-oriented system, a better understanding of a patient’s full care journey has revealed untapped potential for improvements, says Snowden-Bahr, who coauthored the article. To illustrate the challenges, successes and opportunities that can accompany the implementation of global value-based care models, the authors presented two case studies that highlight how Cleveland Clinic established such programs in the US and UAE.
Advertisement
Cleveland Clinic’s Medicare Accountable Care Organization (CCMACO) covers more than 148,000 beneficiaries in northeast Ohio, explains Snowden-Bahr, adding that multidisciplinary care teams form the core of CCAMCO’s outpatient chronic disease management program. Part of the Medicare Shared Savings Program — America’s largest alternative payment model — CCMACO operates within a multidisciplinary system comprising primary care coordinators, population health experts, pharmacists, social workers and other clinicians. The team focuses on reducing unnecessary utilization through the management of care transitions, says Snowden-Bahr.
Lessons learned — Although Cleveland Clinic already had many ingredients of value-based care, the study authors emphasize the complexity of implementing new payment and delivery models. To meet the challenge, CCMACO stakeholders developed governance models, legal arrangements, care teams, and a phased approach for titrating financial risk. In addition, providers and system leaders collaborated to create a formal Quality Committee to better track and evaluate performance based on patient-centric outcomes. Snowden-Bahr says that team-based model used by CCMACO helped to close gaps in the care continuum by focusing on shared goals, such as preventing readmissions through coordinated patient handoffs and improving medication reconciliation through collaborations with pharmacists.
“It’s clear that value-based care models must be patient-centered, with cost, quality and outcomes mediated by the provider-payer relationship,” says Snowden-Bahr, who emphasizes that these interactions are further influenced by the policy and market environment in the provider’s location. “The lessons we learned through our CCMACO care navigation have enabled Cleveland Clinic to develop playbooks for far-reaching success.”
Advertisement
Cleveland Clinic expanded its international footprint in 2015 by opening Cleveland Clinic Abu Dhabi (CCAD). Since its inception, says Snowden-Bahr, the hospital has been focused on introducing technological and clinical innovations for specialties such as cardiac, transplant, and neurological care. To expand coverage for new treatments and service lines and support payment system modernization, he says CCAD collaborated closely with the Departments of Health and Finance, and public and private insurers in the UAE. The study authors assert that CCAD’s rapid growth illustrates the critical role genuine payer-provider partnerships play in an organization’s ability to modernize coverage policies and expand services to meet population needs.
“CCAD was created amidst significant health system reform in the UAE, including the development of mandatory healthcare coverage and the adoption of prospective payment methods,” says Snowden-Bahr. The study authors note that the Emirati population has faced a growing disease burden exacerbated by gaps in specialty care, resulting in increased costs for both payers and the Department of Health. To rectify these problems, CCAD pursued several high-priority reforms, they explain.
Lessons learned — The “secret sauce” of culture and continuous improvement can be difficult to replicate, says Snowden-Bahr, but CCAD remained committed to adopting Cleveland Clinic’s three-pronged culture of patient care, scientific research, and clinical education. Seeding the new system with US leaders and care processes (eg, electronic health record) helped further instill the enterprise-wide “patients first” culture at CCAD.
Advertisement
The NEJM Catalyst article explains how partnerships with payers and ongoing dialogue with regulators have enabled meaningful progress in coding and claims processing, including coverage for germline/somatic testing and pharmacotherapy consultations for heart failure and post-transplant patients. CCAD’s experience also illustrates the importance of coding integrity and a checks-and-balances approach to billing, say the study authors, pointing out that regular engagement among the hospital, its payers and government regulators has also facilitated the development of better cost measurements.
Although the healthcare industry has at least a theoretical commitment to continuous improvement, the study authors say it’s critical to distinguish between value-added activities and those that are value based. Snowden-Bahr explains that value-based care models must be patient-centered – meaning that the cost, quality and outcomes are mediated by the provider-payer relationship. He adds that these interactions are further influenced by the policy and market environment of the provider’s location.
“These case studies illustrate how well-executed partnerships between payers and providers can foster the delivery of value-based care in different clinical and cultural contexts across the globe,” he says. “I believe this patient-centered focus will continue to grow as healthcare reforms accelerate around the world.”
Advertisement
Advertisement

Digital “tripwires” detect and respond to malicious activity, boosting cybersecurity maturity

Thoughtful collaboration, data-driven decisions and effective change management lead to significant savings

Clinical input is integral to technology implementation and adoption strategy

Unit-based project decreases non-urgent alarms

Integrating technology is more than product delivery
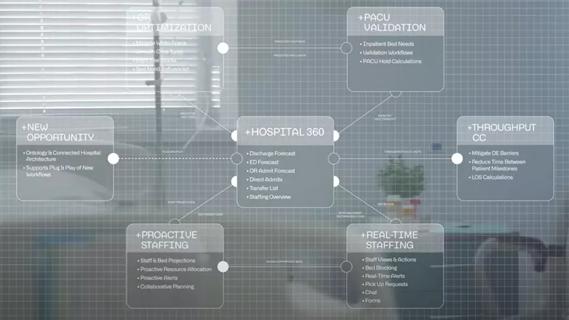
Cleveland Clinic partners with Palantir to create logistical command center

Cleveland Clinic’s roadmap to recovering critical digital assets stems from strategic planning and preparedness

The Friends of Cybersecurity program bridges innovative technology solutions with mitigating security risks