Coping with stress-related disease exacerbations
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The impact of acute and chronic stress from the COVID-19 pandemic will be substantial even in healthy people. Gastroenterologists are very likely to see symptom exacerbations In their patients during this pandemic, but there are ways that providers can help their patients build resilience and reduce the negative impacts of stress. My colleagues and I recently published an article in Current Opinions in Gastroenterology outlining the stress response, how it impacts patients with digestive disease and what providers working with these patients can do to help.
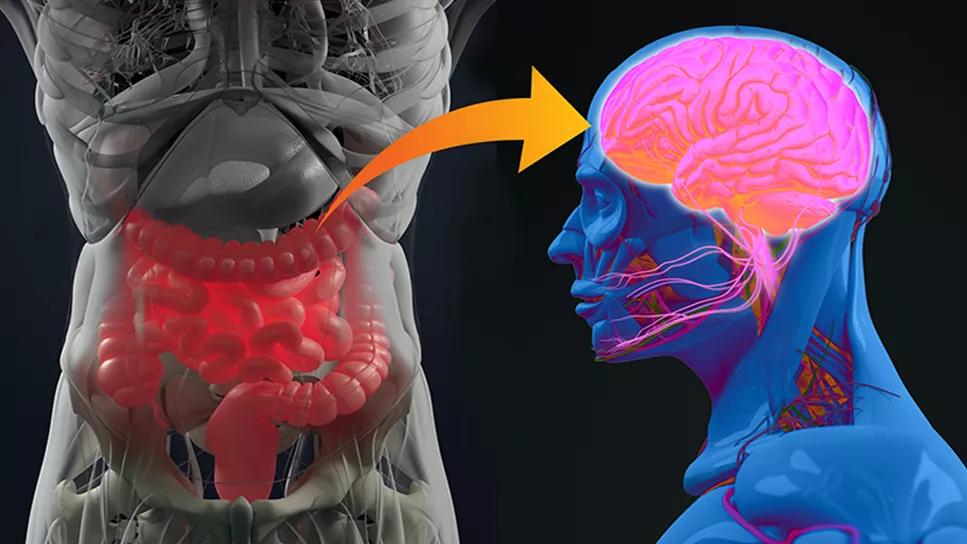
The fight-flight response to stress can, depending on the duration of the response, trigger issues with motility, hunger, satiety and abdominal pain. Our job as we work with patients whose digestive disease is exacerbated by this response is to help them learn to reduce allostatic load, or the adjustments their body must make to return to homeostasis. Some patients with sufficient cognitive and behavioral resources may exhibit resilience, but several behavioral techniques can help people with lower resilience adapt to adversity.
According to the World Health Organization (WHO), psychological first aid includes helping people feel connected to others and a sense of control over the situation as well as ensuring access to appropriate resources. For gastroenterologists, this means providing patients with accurate information about the virus, helping them recognize and utilize available resources, offering alternative ways to connect with people during social distancing and emphasizing routine.
Advertisement
The general adaptation syndrome (GAS) model of stress posits three stages to stress: alarm, resistance and exhaustion. In the alarm stage, the nervous system releases stress hormones to facilitate a fight-flight response. When a stressor is ongoing, like the COVID-19 pandemic, returning to homeostasis is more difficult.
In the second stage — resistance — the individual’s allostatic load ideally returns to baseline. But many patients will not, especially in the prolonged stress of a pandemic. Physicians should consider that patients reporting symptom exacerbations during this time may benefit from stress mitigation techniques, including:
These techniques may replace or augment other pharmaceutical or invasive responses to symptom exacerbation.
In the third stage, called exhaustion, patients become overwhelmed from the ongoing stressor. This is where prolonged dysfunction can occur, and in which identifying a coping strategy becomes more difficult for the patient. Our hope is to intervene during the second stage, when acceptance of behavioral modification is more likely.
Physicians should emphasize the importance of addressing stress with their patients and can offer suggestions, but many patients will need more help. I suggest keeping a referral list of trusted behavioral health professional providers who have experience working with patients with digestive disease. At Cleveland Clinic, our Behavioral Medicine program in the Digestive Disease & Surgery Institute is one of few nationally offering a unique service focused on the gut-brain-body connection as part of patients’ digestive treatment plan. Physicians here can refer patients experiencing stress, behavioral or psychological complaints that cannot be adequately addressed otherwise to a licensed clinical health psychologist who specializes in addressing psychological concerns in patients with digestive disease.
Advertisement
Unfortunately, COVID-19 will likely be with us for a long time, and perhaps will one day become a new normal. For now, the uncertainty, fear and disruption of routine are stressors that can be mitigated through the techniques mentioned above, especially for patients for whom stress exacerbates gastrointestinal disease symptoms.
Dr. Lupe is a clinical health psychologist in the Digestive Disease & Surgery Institute in the Department of Gastroenterology, Hepatology and Nutrition.
Advertisement
Advertisement

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition

As the pandemic evolves, rheumatologists must continue to be mindful of most vulnerable patients

Early results suggest positive outcomes from COVID-19 PrEP treatment

Could the virus have caused the condition or triggered previously undiagnosed disease?

Five categories of cutaneous abnormalities are associated with COVID-19