Groundbreaking study paves way for targeted therapy
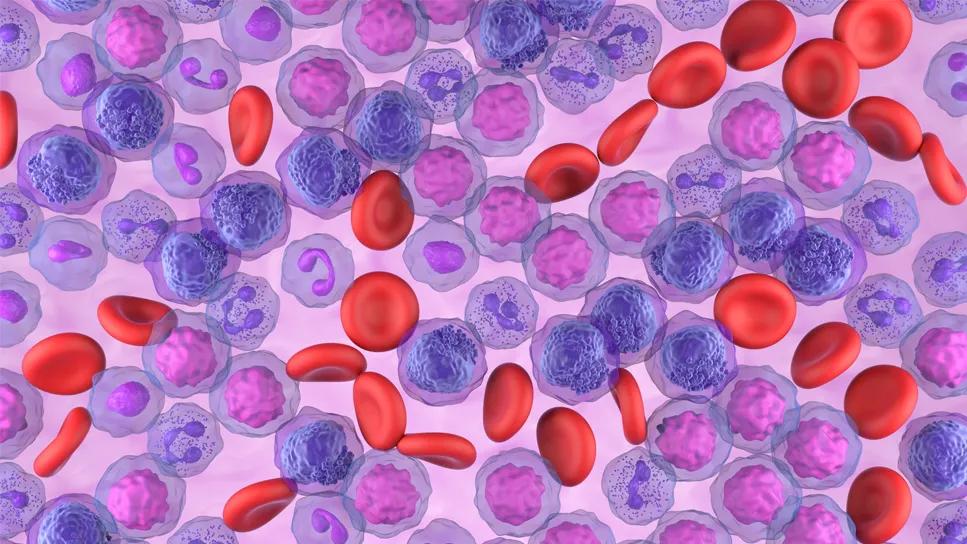
Nucleophosmin (NPM1) is the most frequently mutated gene in de novo acute myeloid leukemia (AML). But just how this mutation causes leukemia has been unknown, until now.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a study recently published in the Journal of Clinical Investigation, authors revealed how NPM1 mutation disrupts the master circuit that makes granulocytes and monocytes, thereby stalling myeloid precursor cells at inherently proliferative points in their maturation course.
“We are most excited because we show how we can turn this information into nontoxic treatment that reverses the mechanism of leukemogenesis. By understanding how myeloid differentiation is blocked, we can unblock it,” says the study’s team lead Yogen Saunthararajah, MD, of Cleveland Clinic Cancer Center. “Our research was done in test tubes and mice, but the drug molecules we used to treat the mice are available for use in clinical trials, and we hope to move forward with such trials soon.”
Using proteomic techniques including mass spectrometry, researchers identified the molecular machinery within myeloid cells in which NPM1 participates. They found:
Advertisement
“In brief, we discovered that mutant NPM1 disrupts the PU.1/CEBPA/RUNX1 master circuit to repress instead of activate granulomonocyte lineage programs,” says Dr. Saunthararajah. “Maturation is the usual cue to stop replicating. Because these cells don’t mature, they continue to replicate, causing AML.”
Can these leukemogenic actions of mutant NPM1 somehow be reversed? That was the next step for the research team. Using in vitro and in vivo models, they discovered that:
“When used together, the clinical small molecules selinexor and decitabine extended survival of mice with leukemia by more than 160 days, compared to mice that didn’t receive the drugs,” says Dr. Saunthararajah.
Advertisement
These findings open the door to noncytotoxic differentiation-restoring treatments for patients with NPM1-mutated AML, says Dr. Saunthararajah.
NPM1 mutation is present in approximately 30 percent of AML cases. With current antimetabolite/cytotoxic treatments, only about 50 percent of these patients have long-term survival, he notes.
“There have been no targeted therapies for NPM1-mutated AML because, until now, we didn’t fully understand how mutant NPM1 was leukemogenic,” says Dr. Saunthararajah. “The results of our study can bring new hope of targeted or precision non-cytotoxic treatments for the many patients with chemorefractory, NPM1-mutated AML.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient