12 reasons people give for not wanting the influenza vaccine

By Sherif Beniameen Mossad, MD, FACP, FIDSA, FAST*
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Please note: this is an abridged version of an article originally published in the Cleveland Clinic Journal of Medicine.
The benefits of influenza vaccination are clear to those in the medical community. Yet misinformation and unfounded fears continue to discourage some people from getting a flu shot. During the 2018–2019 influenza season, only 45% of US adults and 63% of children were vaccinated.
What should we tell patients who say no to the flu shot? Here are 12 reasons people give for not wanting to receive the inactivated influenza vaccine, along with some potential responses and comments about the nasal live attenuated vaccine.
Advertisement
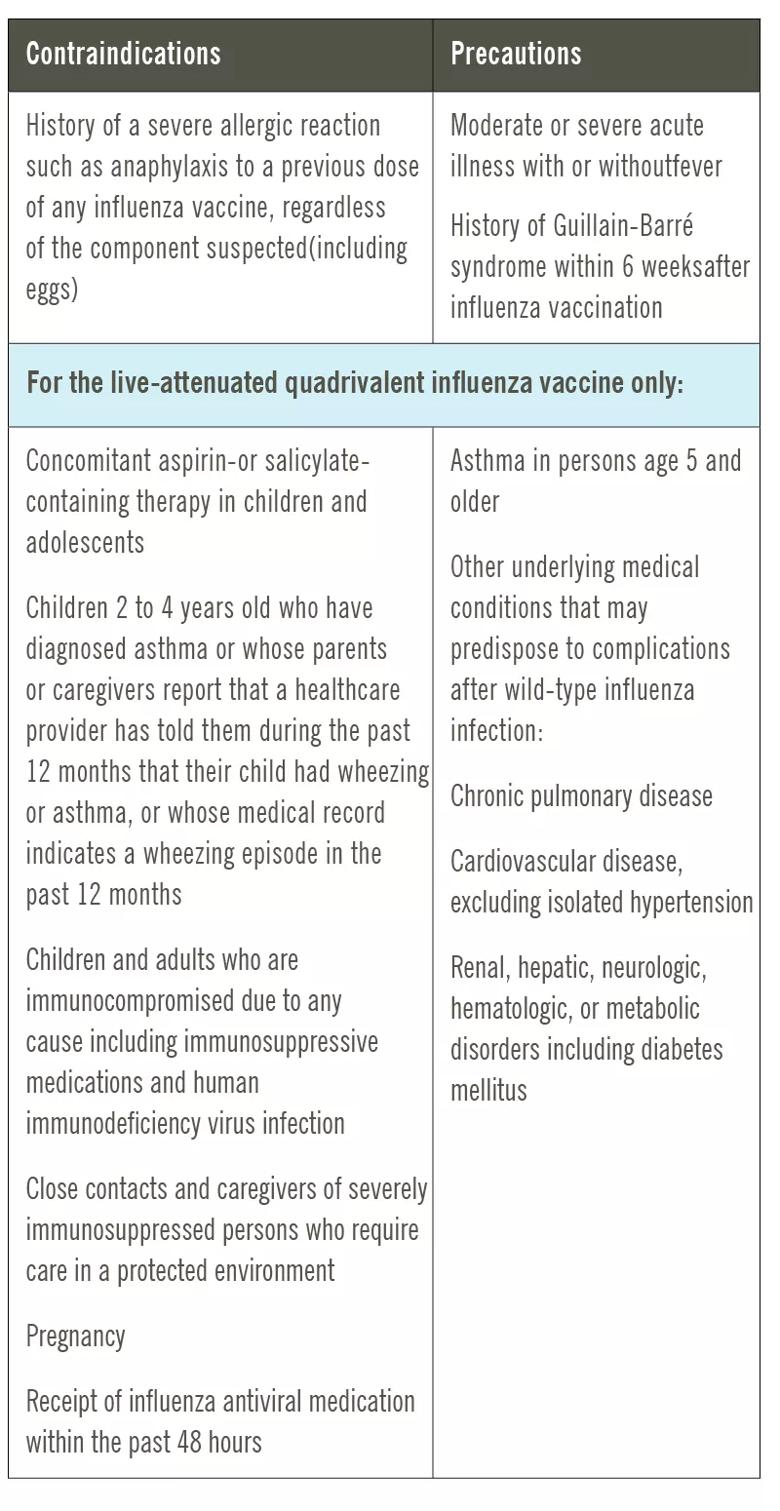
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/495e58ec-4aea-4e3e-95d4-df73eb5acacc/20-CCC-1853143-FluVaccineDoubters-contraindctn-table-800x1550-1_jpg)
Healthcare providers should try to understand the public’s misconceptions about seasonal influenza and influenza vaccines in order to best address them.
Advertisement
Advertisement

Emerging evidence suggests a patient-specific approach

Not if they meet at least one criterion for presumptive evidence of immunity

Essential prescribing tips for patients with sulfonamide allergies

Confounding symptoms and a complex medical history prove diagnostically challenging

An updated review of risk factors, management and treatment considerations

OMT may be right for some with Graves’ eye disease

Perserverance may depend on several specifics, including medication type, insurance coverage and medium-term weight loss

Abstinence from combustibles, dependence on vaping