It’s safe and accurate, but who should be tested?
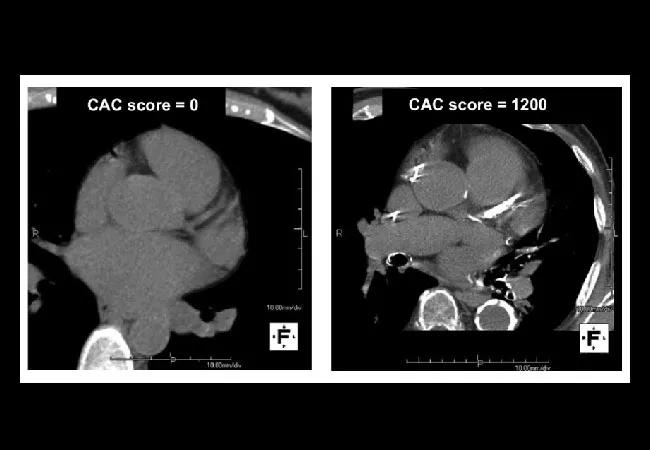
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b7b5b34c-0ec4-44d6-b048-a70de87ded29/18-CCR-5881-calciumScoreHV-2-650x450_jpg)
18-CCR-5881-calciumScoreHV-2-650×450
By Michael B. Rothberg, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 1984, Jim Fixx, who wrote The Complete Book of Running,1 went out for his daily run and died of a massive heart attack. He was 48. Unbeknownst to him, he had three-vessel coronary artery disease.
His case illustrates the difficulty of diagnosing coronary artery disease in patients who have no symptoms of it. For many, the initial presentation is myocardial infarction or death. Until recently, there was no reliable way to diagnose subclinical coronary artery disease other than angiography, and there is still no way to rule it out. As a result, physicians have concentrated less on diagnosing subclinical disease and more on assessing the risk of myocardial infarction.
The risk factors for coronary artery disease (age, male sex, smoking, hypertension and cholesterol) have been well known for half a century. By combining risk factors with the appropriate weighting, it is possible to predict an individual’s risk of a myocardial infarction.
In 2013, the American College of Cardiology/American Heart Association (ACC/AHA) guidelines applied this risk-based approach to prescribing statins for primary prevention.2 Instead of focusing on low-density lipoprotein cholesterol concentration, which by itself is a poor predictor of myocardial infarction, they recommended using the Pooled Cohort Equation3 to determine the risk of a cardiovascular event within 10 years. For patients at high risk (> 7.5 percent), the benefits of a statin generally outweigh the harms. For those at low risk (< 5 percent), the opposite is true. For patients in between, there is room for shared decision-making.
Advertisement
Debate has focused on the predictive accuracy of the equation, the threshold for treatment and the fact that almost all men over 60 qualify for treatment.4 These objections stem from the focus on risk rather than on diagnosis of the underlying disease.
Because one-third of “high-risk” patients never develop cardiovascular disease,5 the risk-based approach necessitates overtreatment. Those without disease cannot benefit from treatment but nonetheless suffer its side effects, cost and inconvenience. Raising treatment thresholds (e.g., treating only patients whose 10-year risk exceeds 10 percent) improves the ratio of patients with disease to those without but also misses diseased patients who have few risk factors. “Low risk” is not “no risk.”
Diagnostic testing is preferred if such testing is safe and inexpensive.
In the September 2018 issue of Cleveland Clinic Journal of Medicine, Parikh and colleagues6 review coronary artery calcium scoring, a diagnostic test for coronary artery disease. They conclude that calcium scoring is strongly predictive but should be reserved for patients at intermediate risk, to help them decide about treatment [see this Consult QD post excerpting the portion of their review focusing on recommendations]. This is clearly the right approach, but the authors leave the term “intermediate” undefined, and their clinical examples offer too little guidance as to where the borders lie.
The ACC/AHA guidelines specify a narrow intermediate range (5.0 to 7.4 percent). For patients in this risk range, calcium scoring could reclassify most as being at high or low risk, helping to clarify whether statins are indicated.
Advertisement
However, only 12 percent of patients fall into this category.7 What about patients at higher risk? Could they be reclassified as being at low risk if their calcium score was 0?8 Conversely, could some low-risk patients discover that they are at high risk and perhaps take action?
The ACC/AHA guidelines recommend against calcium scoring in these circumstances. One concern was that calcium scoring had not been tested with the Pooled Cohort Equation. Another concern related to cost and radiation exposure, but as Parikh and colleagues point out,6 the cost has now fallen to less than $100, and radiation exposure is similar to that with mammography.
Who, then, should we test? For patients at high or low risk according to the Pooled Cohort Equation, two questions determine whether calcium scoring is warranted: How much would an extremely high or low score (i.e., 0 or > 400) change the risk of an event, and how likely is an extreme score?
The first question relates to the usefulness of the test, the second to its cost-effectiveness. If even an extreme score cannot move a patient’s risk into or out of the treatment range, then testing is unwarranted. At the same time, if few patients have an extreme score, then the cost per test that changes practice will be high.
Because calcium scoring is a direct test for disease, it is extremely predictive. When added to risk-factor models, it substantially improves discrimination9 and exhibits excellent calibration.10 This is true whether the outcome is a major cardiovascular event or death from any cause.
Advertisement
But the calcium score is not strong enough to override all other risk factors. A patient with a predicted 10-year risk of 18 percent according to the Pooled Cohort Equation and a calcium score of 0 could be reclassified as being at low risk, but a patient with a 10-year predicted risk of 35 percent could not. The same is true for patients at low risk. A patient with a 4 percent risk and a calcium score higher than 400 would be reclassified as being at high risk, but not a patient with a 1 percent risk.
Extreme calcium scores are common, especially in patients at high risk. In the Multi-Ethnic Study of Atherosclerosis (MESA) cohort, 45 percent of patients with a 10-year predicted risk of 7.5 percent to 20 percent had a calcium score of 0, reclassifying them into the low-risk category.11 Even if the predicted risk was greater than 20 percent, 1 in 4 patients had a score of 0. In contrast, if the 10-year predicted risk was below 5 percent, one-fifth of patients had a calcium score greater than 0, but only 4 percent had a score greater than 100.
Nevertheless, patients in the low-risk category whose baseline risk is close to 5 percent may wish to undergo calcium scoring, because a positive test opens the door to a potentially lifesaving treatment. In general, the closer patients are to the treatment threshold, the more likely they are to be reclassified by calcium scoring.
The Society for Cardiovascular Computed Tomography currently recommends coronary artery calcium scoring for patients whose 10- year risk is between 5 percent and 20 percent.12 These numbers are easy to remember and a reasonable approximation of the number of patients likely to benefit from testing.
Advertisement
Primary care physicians interested in more exact personalized medicine can use a risk calculator derived from the MESA cohort.13 Based on 10-year outcomes for 6,814 participants, Blaha and colleagues8 derived and validated this risk-prediction tool incorporating all the elements of the Pooled Cohort Equation in addition to family history, race and calcium score.
The tool offered good discrimination and calibration when validated against two external cohorts (the Heinz Nixdorf Recall Study and the Dallas Heart Study).10 The C statistics were 0.78 and 0.82, with 10-year risk predicted by the tool within half a percent of the observed event rate in each cohort.
The online calculator displays the 10-year risk based on risk factors alone or including a calcium score, allowing the clinician to gauge the value of testing. For example, a 70-year-old nonsmoking white man with a total cholesterol level of 240 mg/dL, high-density lipoprotein cholesterol of 40 mg/dL and systolic blood pressure of 130 mm Hg on amlodipine has a 15.2 percent 10-year risk (well above the 7.5 percent threshold for statin therapy). However, if his calcium score is 0, his risk falls to 4.3 percent (well below the threshold). Sharing such information with patients could help them to decide whether to undergo coronary artery calcium scoring.
Ultimately, the decision to take a statin for primary prevention of coronary artery disease is a personal one. It involves weighing risks, benefits and preferences. Physicians can facilitate the process by providing information and guidance. Patients are best served by having the most accurate information. In many cases, that information should include calcium scoring.
This article is reprinted from the September 2018 issue of Cleveland Clinic Journal of Medicine (2018;85:717-719).
Dr. Rothberg is Vice-Chair for Research and Director, Center for Value-Based Care Research, in Cleveland Clinic’s Medicine Institute.
Advertisement
Emerging evidence suggests a patient-specific approach
Not if they meet at least one criterion for presumptive evidence of immunity
Essential prescribing tips for patients with sulfonamide allergies
Confounding symptoms and a complex medical history prove diagnostically challenging
An updated review of risk factors, management and treatment considerations
OMT may be right for some with Graves’ eye disease
Perserverance may depend on several specifics, including medication type, insurance coverage and medium-term weight loss
Abstinence from combustibles, dependence on vaping