Pinpoint control, high magnification and minimal invasiveness
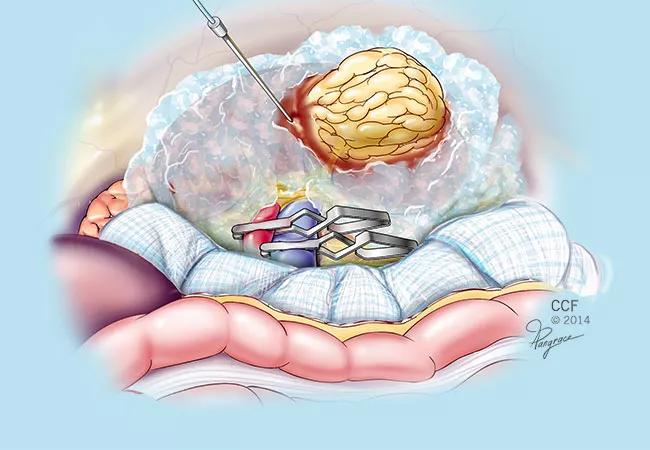
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e2d6b294-c070-4a78-a3db-96947b20a2d4/650x450-NEPHRECTOMY-ice_corporeal-renal-cooling-80555-_jpg)
650×450-NEPHRECTOMY-ice_corporeal-renal-cooling-80555-
Urologic surgeons are using robot-assisted systems in increasingly complex cases due to the equipment’s pinpoint control, high magnification and minimal invasiveness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
One such application is partial nephrectomy (PN), where the robot’s precision aids removal of large, deeply infiltrating renal tumors while enabling surgeons to spare valuable nephrons.
To ensure proper visualization of the surgical field during PN, the renal hilum must be temporarily clamped. “Cooling the kidney to temperatures of 10°-20°C allows for more prolonged clamp times which can be very helpful for complicated excisions. Our experience with over 5,000 partial nephrectomies suggests that hypothermia provides the strongest and most consistent protection against irreversible ischemic injury,” says urologist Steven Campbell, MD, PhD.
Maintaining adequate renal hypothermia while protecting adjacent bowel can be difficult in minimally invasive settings. In 2003, Cleveland Clinic surgeons were the first to perform laparoscopic PN using ice slush.
In 2014, they introduced a novel, easily reproducible robotic PN intracorporeal renal hypothermia technique employing ice slush. In 2016, the surgeons continued to refine this technique and gained experience, having performed about 40 procedures to date.
“We developed a cost-effective, minimally invasive approach with minimal additional morbidity to the patient,” says Jihad H. Kaouk, MD, the Urological & Kidney Institute’s Vice Chair for Surgical Innovations and Director of the Center for Robotic and Image-Guided Surgery.
The sterile ice slush used in the robotic PN procedure is preloaded into modified 20 mL syringes and injected into the abdomen and packed around the kidney via a lateral 12 mm accessary port. Approximately half a liter of slush can be introduced within five minutes and achieves consistent renal cooling in the range of 15°C. A laparoscopic sponge is placed around the kidney as a thermal barrier to protect nearby intestine. Renal and core body temperatures are monitored during the procedure. After tumor excision and renorrhaphy, the remaining slush is suctioned or placed along with the specimen in an entrapment sac.
Advertisement
“Intracorporeal ice cooling of the kidney allows the surgeon more time to cut out complex kidney tumors and reconstruct the kidney,” Dr. Kaouk says. “This technique is not for every case, but is beneficial whenever ischemia time is anticipated to be longer than 25 minutes.”
The team analyzed the postoperative renal function of patients with similar preoperative estimated glomerular filtration rates (eGFR), tumor size and complexity who underwent robotic PN using either cold or warm ischemia.
The comparison showed that ice slush robotic PN was associated with a 12.9 percent greater preservation of eGFR in the short-term (one- to three-week) postoperative period. There was no difference in eGFR between the cold and warm ischemia cohorts after six months. Additional research will better define icing’s short- and long-term impacts, Dr. Kaouk says.
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key