No actionable pathology was missed in large patient series
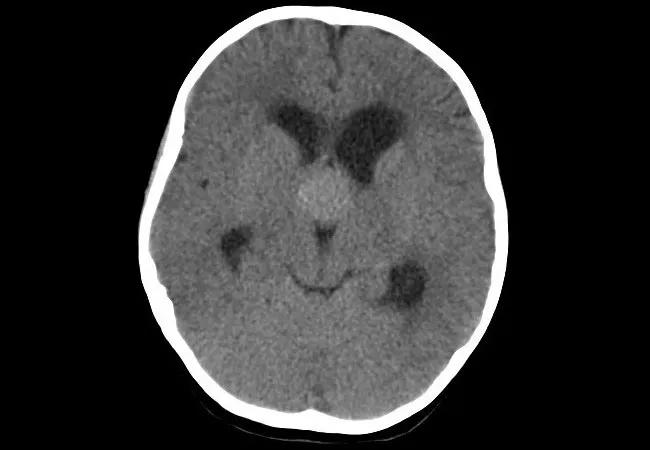
For children who present with papilledema and no red flags for underlying tumor or thrombosis, imaging by CT alone — without MRI follow-up — may be adequate. That’s the conclusion of a review of CT and MRI findings among a series of Cleveland Clinic pediatric patients who were diagnosed with papilledema, idiopathic intracranial hypertension, brain tumor or cerebral venous thrombosis. The research was presented at the 2020 virtual meeting of the American Academy of Neurology this spring.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“MRIs are costly and often require general anesthesia in children, so avoiding them when they are not essential reduces needless expense and risk,” says senior author Gary Hsich, MD, a pediatric neurologist in Cleveland Clinic’s Center for Pediatric Neurosciences. “Our data support the notion that, in select children with papilledema — i.e., those with a normal neurologic examination — CT provides adequate imaging evaluation.”
Papilledema, a sign of increased intracranial pressure, can be found serendipitously in children during a routine eye check or during evaluation for vision changes, headaches or nausea. Although brain MRI is often performed to rule out underlying brain tumor or cerebral venous thrombosis, few data exist, especially in the pediatric population, to support the necessity of MRI over CT to diagnose these rare entities.
Cleveland Clinic medical records from 2012 to 2019 were reviewed for patients aged 18 years or younger with a diagnosis of either papilledema/optic disc edema, brain tumor, cerebral venous thrombosis or idiopathic intracranial hypertension. [Editor’s note: The numbers reported below reflect the actual study presentation, which included data for a few more patients than in the abstract published in the AAN meeting proceedings.]
The following two overlapping groups were analyzed:
1) Patients who presented with papilledema and otherwise normal neurologic evaluation (n = 142). CT and MRI results were reviewed to compare diagnostic findings. Imaging results were as follows:
Advertisement
2) Patients (with or without papilledema) diagnosed with brain tumor or cerebral venous thrombosis (n = 118). Of this group, 69 patients underwent brain CT. These patients’ clinical presentation and imaging findings were reviewed, with the following results:
“For everyone in the series, brain tumors or thrombi were either discovered by CT or suspected clinically, prompting additional examination,” notes study co-author and presenter Travis Larsh, MD, a fellow in child neurology at Cleveland Clinic.
“Most physicians order an MRI for children who present with papilledema out of fear of missing something,” says Dr. Hsich. “This study provides support that CT can be adequate in a child with normal neurologic findings.”
Both Drs. Hsich and Larsh say that in their own practices, they will be more mindful when considering whether an MRI is needed for children presenting with papilledema. They hope this study will provide other pediatric neurologists with the confidence to do the same, but they aren’t certain that will happen.
“It’s difficult to decide not to avail our patients of the best technology,” says Dr. Larsh. He adds that conducting research to prove a negative — in this case, that there is no actionable finding — is especially difficult. “But one must also consider the risks and costs, and prescribe tests only when there is reasonable evidence that something new will be uncovered.”
Advertisement
To overcome any inertia, Drs. Hsich and Larsh call for similar analyses of data from other institutions to either support or refute their findings.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help