Benefits include swifter patient transport, more on-time starts for cardiovascular procedures

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bb21e97d-5010-4af7-8271-50f8a25a6641/23-HVI-4078942-CQD-650x450-1_jpg)
Medical team pushing hospital bed down corridor
Efficiency is a high priority for healthcare organizations in terms of optimizing resources, standardizing processes, and promoting patient and caregiver experience while maintaining high quality and safe patient care. Analyzing operational data to assess workflow efficiency may uncover process issues. A multidisciplinary team approach to identifying challenges, determining solutions and implementing change, with use of continuous improvement (CI) methodology, aims to achieve successful, sustainable outcomes. This was the result at Deborah Health and Lung Center following a collaborative CI project with Cleveland Clinic’s Heart, Vascular & Thoracic Institute (HVTI) Advisory Services team.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Deborah Heart and Lung Center (DHLC) is an 89-bed specialty teaching hospital in Browns Mills, New Jersey, that began an alliance relationship with Cleveland Clinic’s HVTI in 2019. Under this relationship, Cleveland Clinic HVTI’s Advisory Services team works with DHLC to build upon existing high-quality outcomes, optimize efficient resource allocation, develop and enhance existing programs, and expand services. DHLC leaders and the Advisory Services team recognized an efficiency opportunity for the outpatient procedure unit (OPPU) and embarked on a structured CI project to achieve sustainable results.
The OPPU serves as the entry point for patients coming to the facility for outpatient procedures. Patients who arrive at the OPPU will eventually move to the cardiac catheterization lab, electrophysiology (EP) lab or cardiovascular operating rooms (ORs) for their procedures. Unlike procedures in the cath and EP labs, procedures for vascular surgery cases were identified as not consistently starting on time. The team observed that only 67% of vascular surgery cases started on time for the period of January through July 2022. The DHLC team performed an internal review of reasons for the delays, identifying several possible causes.
DHLC’s leadership team sought to partner with Cleveland Clinic’s HVTI Advisory Services team to fully address the issues.As part of an improvement initiative, the team engaged with DHLC’s direct clinical caregivers to help them with the CI tools and techniques needed to reach their goals.
Advertisement
HVTI’s Advisory Services team began the engagement by working with the DHLC team to thoroughly define the issues and the reason that change was important to service line success. While the impetus for the project was delays in on-time starts for DHLC’s vascular ORs, the multidisciplinary team realized that the OPPU provides pre-procedural care for multiple specialties. As a result, improving operational efficiencies for the OPPU required examining multiple factors. Comprehensive data analysis conducted by the Cleveland Clinic team demonstrated key triggers for the delays in patient arrival time to the OR, including processes around obtaining informed consent, patient arrival times, variability in case scheduling and late changes/add-ons, transportation, and patient preparation time. Consequently, the team readjusted its focus to improve efficiencies for the OPPU by standardizing processes that would help not only the vascular ORs but the other procedural areas as well.
The recommended process changes were:
The team also conducted initial analysis to define baseline metrics and set targets for future performance in the OPPU. These metrics included:
Advertisement
DHLC’s OPPU team used a plan-do-check-act (PDCA) approach to enhance communication between the OPPU, procedure areas and ORs with use of an electronic patient tracking board. PDCA is an iterative approach to problem solving in which teams develop their initial improvement opportunities, implement plans to address those opportunities, verify the impact of implementation and then act to improve based on what they learned from implementation.
The electronic tracking board is visible to caregivers in the procedural areas. Prior to this initiative, the cath lab, EP lab and OR teams were not aware when a patient’s preparation was complete and the patient was ready for transport from the OPPU to the procedural area. The team recognized an opportunity to improve electronic communication between the OPPU and the procedural areas and enlisted the support of DHLC’s nursing informatics specialist. Nursing informatics helped the OPPU create a “ready” indicator on the patient tracking board to identify when patients were prepared for their procedure. The visible icon notifies the receiving department that the patient is ready for transport. The procedural/OR team then transports the patient from the OPPU to the procedural area if they have completed their patient preparatory work. This follows CI best practices in which work is pulled from one area to another rather than being pushed onto another department. This allowed the procedural/OR teams to transport patients from the OPPU as space in each procedural area became available.
Advertisement
Use of the electronic patient tracking board as a communication mechanism quickly had an impact on the efficiency of patient transport from the OPPU to the procedural areas. “It has made quite a difference in our ability to enhance efficiency in the OPPU and meet our goal of first-case on-time starts,” says Geralyn Angelo, RN, Director of Medical-Surgical Nursing Services at DHLC.
The HVTI and DHLC teams then collaboratively developed a completion plan to help the OPPU team ensure its desired performance metrics and targets were maintained. A well-defined completion plan enables achievement of project goals by defining the tasks required for success and identifying specific individuals responsible and accountable for achieving the outcomes. The final completion plan is a comprehensive list with established due dates that match tasks with the accountable individuals.
The DHLC team members achieved their target performance metrics within the first 60 days after implementing changes, as shown in the table. After 90 days, the team was still performing above its baseline performance. On-time starts for cardiothoracic ORs improved from 82% to 94% and vascular from 67% to 79%. Other key metrics also demonstrated improvement in team performance.
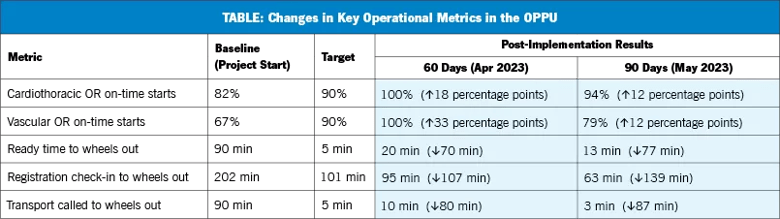
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f52f7759-f4aa-4ff1-8237-8fd14ea2a0bc/23-HVI-4078942-805x-OPPU-chart_png)
The DHLC team developed a group text thread with the transport director that allowed communication of the OPPU schedule 24 hours in advance, and the OPPU and procedural teams implemented a small group meeting to plan staffing and resources. These two changes helped drive the improvements noted in the table.
Advertisement
“We solve issues in real time between the OR, OPPU and transport leadership. There is no need for an additional meeting,” observes Ms. Angelo. “It has been a pleasure working with Cleveland Clinic’s Advisory Services team. Timely responses and recommendations for continuous improvements have allowed our OPPU team to achieve first-case on-time starts.”
“This engagement between DHLC and HVTI’s Advisory Services team demonstrated the effectiveness of Cleveland Clinic’s structured approach to continuous improvement,” says Suma Thomas, MD, MBA, Vice Chair, HVTI Strategic Operations. “This approach enables team members to enhance all aspects of care, including operational efficiencies, patient safety, quality, patient experience and caregiver experience.”
For information on affiliation or alliance opportunities with Cleveland Clinic’s Heart, Vascular & Thoracic Institute, visit clevelandclinic.org/hvtiadvisoryservices or email Amanda Lesesky at leseska@ccf.org.
Advertisement
Digital “tripwires” detect and respond to malicious activity, boosting cybersecurity maturity
Thoughtful collaboration, data-driven decisions and effective change management lead to significant savings
Clinical input is integral to technology implementation and adoption strategy
Unit-based project decreases non-urgent alarms
Integrating technology is more than product delivery
Cleveland Clinic partners with Palantir to create logistical command center
Cleveland Clinic’s roadmap to recovering critical digital assets stems from strategic planning and preparedness
The Friends of Cybersecurity program bridges innovative technology solutions with mitigating security risks