Note: This article is reprinted from Cardiac Care: An Update for Physicians from the Heart, Vascular and Thoracic Institute (Spring 2024)
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Until recent years, open carotid endarterectomy (CEA) has been the standard of care for many patients with severe or symptomatic carotid stenosis. However, minimally invasive procedures such as transfemoral carotid stenting and now transcarotid artery revascularization (TCAR) have emerged as safe and effective minimally invasive alternatives for patients with carotid disease. The Department of Vascular Surgery at Cleveland Clinic in Florida provides multispecialty care and access to the industry’s most advanced technology and procedures, which now includes the use of TCAR for many patients in need of carotid interventions.
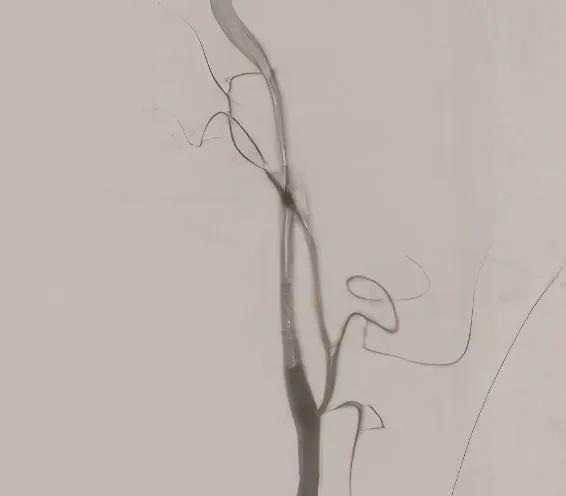
TCAR is a less invasive, clinically proven, approved treatment option for carotid artery disease. The procedure begins with a small incision just above the clavicle. A temporary sheath is placed directly into the carotid artery in an area away from the disease. The sheath connects to a filter and flow reversal system outside of the body and then to another small sheath that is placed directly into the femoral vein. The difference in pressure causes the reversal of blood flow away from the brain, decreasing the risk of a stroke. A stent is then inserted through the sheath to open the stenotic and diseased carotid artery. Because of the blood flow reversal, any debris that might break loose during stent placement won’t travel up to the brain, rather it travels downward and gets trapped in the filter, and the filtered blood returns into the vein.
The postoperative course is very important for faster recovery after carotid surgery. Close coordination of care with the ICU team focusing on adequate hemodynamic support including strict blood pressure management, makes a substantial difference in the patient’s recovery. Patients can expect to go home within 24 hours of the procedure.
Advertisement
When compared to traditional open CEA, studies have shown that patients undergoing TCAR usually recover quickly with less pain and smaller scars. TCAR patients also have a lower risk of cardiac complications, myocardial infarction and cranial nerve injury, and have a shorter procedure time when compared to open CEA.
Proper selection and identification of patients who are candidates for TCAR is critical. TCAR is now available for patients of all risk levels, including those with symptomatic and severe asymptomatic carotid stenosis as well as high anatomical or medical risk for open surgery.
Since 2022, Cleveland Clinic Weston Hospital has performed TCAR routinely using a minimally invasive approach. Our center performs the highest volume of TCARs in South Florida. Outcomes have been excellent, with a 100% technical success rate and no reported strokes for our patients. Our expertise in open vascular surgery and CEA combined with newer, advanced endovascular techniques such as TCAR, has translated into the best possible patient outcomes.
Dr. Sasson is a vascular surgeon with Cleveland Clinic Weston Hospital and serves as Co-Director of Cleveland Clinic’s Vein Center in Florida.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.