An innovative hybrid treatment that combines minimally invasive epicardial and endocardial ablation to achieve rhythm control in persistent and long-standing persistent atrial fibrillation (AF) is gaining traction as the incidence and prevalence of AF rises nationally.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
At least 2.7 million Americans currently live with AF, the most common heart arrhythmia. This number is expected to increase dramatically as the U.S. population ages.
About 30% of cases are paroxysmal AF, lasting less than 7 days before resolving spontaneously. The remaining 70% are cases of persistent AF, lasting at least 7 days, or long-standing persistent AF, with symptoms lasting for more than a year.
The Convergent procedure requires a multidisciplinary approach to combine surgical epicardial ablation with catheter endocardial ablation. It was added to the 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation published last November.
Inclusion of the two-step treatment is largely based on the results of the CONVERGE trial, which found it to be more effective than catheter ablation alone. In the trial, 67% of patients in the combo arm were free of AF one year later versus 49% in the catheter ablation arm.
Luis Velazco-Davila, MD, a board-certified thoracic and cardiovascular surgeon with Cleveland Clinic Indian River Hospital in Vero Beach, Florida, and Brett Faulknier, DO, Director of Electrophysiology at Indian River Hospital, offer this innovative treatment for patients with persistent and long-standing persistent AF who have not had success with medication or previous ablation treatments. The procedure is also available at Cleveland Clinic Weston Hospital.
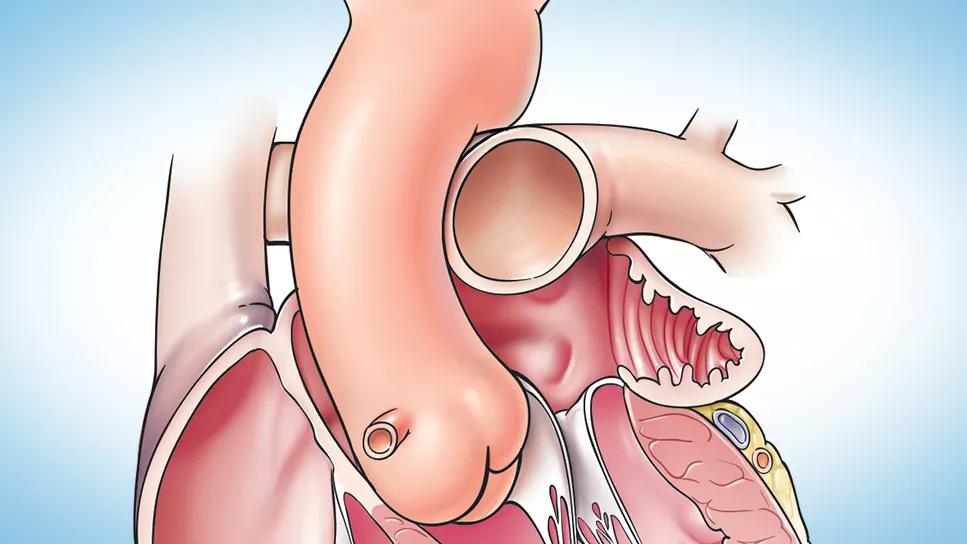
Epicardial ablation is the first step of the Convergent procedure. Dr. Velazco makes a small subxiphoid incision (2.5-3 cm) just below the rib cage. A cannula is then threaded around the heart to the posterior wall of the left atrium, providing access for a device used to deliver radiofrequency (RF) energy.
Advertisement
Under endoscopic visualization, lesions are created on the surface of the heart to block arrhythmogenic electrical activity. In addition to isolating the pulmonary veins, known foci for AF inducing signals, Dr. Velazco creates parallel rows of lesions along the left atrial posterior wall.
“Studies have shown that pulmonary vein isolation alone is less effective for restoring sinus rhythm for persistent forms of AF,” Dr. Velazco explains. He also notes that by directing RF energy from the outside of the heart inward, there is far less risk of damaging nearby structures, including the esophagus and phrenic nerve.
Following the 2 to 3 hour surgery, most patients will have an overnight hospital stay and will be back to normal activity in about a week.
About a month later, Dr. Faulknier conducts the second step of the Convergent procedure. Using a catheter-approach through a groin vein, he performs endocardial ablation to complete the lesion set and electrically isolate the pulmonary veins and posterior wall.
“Patients with persistent AF tend to have larger atria with thicker posterior walls, which make them harder to ablate from the inside alone,” explains Dr. Faulknier. “Endocardial mapping allows me to target and accurately line up the endo scarring to achieve transmural penetration and lower the risk of AF recurrence.”
Following catheter ablation, a majority of patients are able to go home the same day, though some may be required to stay overnight depending on their general state of health or other factors.
Advertisement
“The Convergent procedure is safe and effective,” says Dr. Faulknier. He also points to studies, including the CONVERGE trial, where patients have reported feeling better both physically and emotionally after treatment.
When paroxysmal AF becomes persistent, the heart cannot return to a normal rhythm without treatment. It is a progressive condition that may become permanent or lead to severe complications such stroke and heart failure. Clinical guidelines recommend early detection and treatment with a new emphasis on early rhythm control.
“The longer persistent AF goes without treatment, the harder it is to manage,” stresses Dr. Faulknier. “Our team is excited to offer this new approach for a select group of our atrial fibrillation patients who previously may have been selected for a rate control option only.”
Convergent is recommended when antiarrhythmic drugs are not working or cannot be tolerated by the patient. Contraindications include previous heart surgery with existing scar tissue or an intolerance for anesthesia or intubation. Some individuals with a very long history of AF may be excluded, as well.
“Combining a minimally invasive surgical treatment with catheter ablation allows us to provide a durable result, and a lot of patients can benefit from this approach,” adds Dr. Velazco. He recommends referring patients with AF to an electrophysiologist as early as possible for an evaluation.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.