Note: This article is reprinted from Cardiac Care: An Update for Physicians from the Heart, Vascular and Thoracic Institute (Spring 2024)
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Surgical myectomy is one of the oldest open-heart procedures. It was introduced in the 1960s by Andrew Glenn Morrow, MD, to remove a limited segment of myocardium from the proximal anterior ventricular septum. The procedure has evolved to allow for a more extended distal resection of hypertrophic myocardium with low operative risks and excellent clinical outcomes.
Surgery for hypertrophic obstructive cardiomyopathy (HOCM) reliably reverses disabling heart failure by permanently abolishing mechanical outflow impedance and mitral regurgitation, resulting in normalization of left ventricular pressures and preserved systolic function.
Perioperative mortality for myectomy has declined to 0.6% in experienced institutions, making it one of the safest open-heart procedures currently performed. Extended myectomy relieves symptoms in >90% of patients by ≥ 1 NYHA functional class, returning most to normal daily activity.
Patients with HOCM are considered for surgical intervention when they have poor exercise capacity for their age (usually NYHA class III/IV), when they develop symptoms not responsive to medical treatment or cannot tolerate medical treatment, and present LV outflow gradient ≥ 50 mmHg by echocardiography at rest or with physiologic exercise provocation.
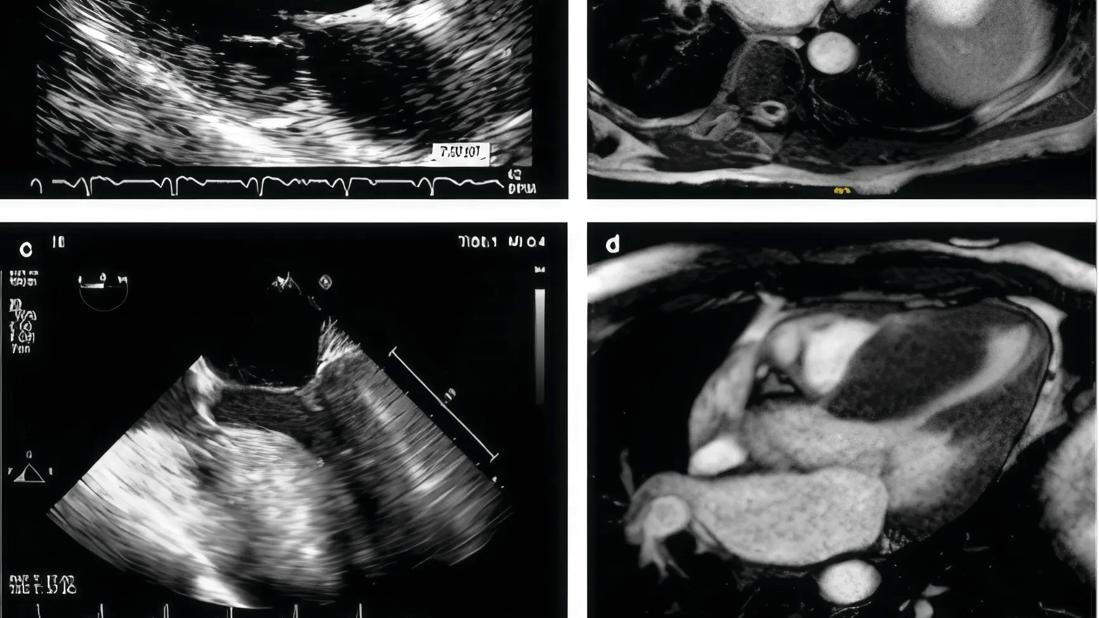
There are infinite configurations of the septum (Figure 1). Cleveland Clinic surgeons review all preoperative imaging studies, including magnetic resonance imaging and echocardiograms, and occasionally can print a 3-dimensional model of the patient’s heart to understand the anatomy.
Advertisement
The operation is carried on through an incision of the initial portion of the aorta that allows to retract the aortic valve leaflets and provide exposure of the complex inner anatomy of the left ventricle including the interventricular septum, the papillary muscles with their chordae, and the mitral valve. Long-toothed forceps and scalpel are used to perform a tailored resection of septal myocardial muscle that starts about 15 mm below the right coronary cusp, away from the membranous septum and the bundle of His, extending longitudinally towards the apex and tapering down laterally as the resection ends in the regions of normal myocardial thickness (Figure 2).
The resected myocardial muscle is placed over a towel, in exactly the location it was removed, to allow the surgeon to estimate the residual septal thickness by subtracting the thickness and length of the
resected muscle from the mental 3D image formed during baseline assessment. A standard myectomy excises approximately 8 g of muscle (Figure 3), although some cases will require resection of up to 20 g of muscle.
We will frequently have our dedicated hypertrophic obstructive cardio-myopathy cardiologist in the operating room to discuss the results of the operation, and a functional test is performed at the end of the operation by administration of isoproterenol to produce a transient hyperdynamic state that would produce obstruction and reveal any residual hypertrophy.
Additional procedures, such as realignment of the papillary muscles, might be required in selected patients with mid-cavitary obstruction. These procedures are further tailored to specific disposition of the papillary muscles and mitral sub-valvular apparatus.
Advertisement
Surgery for HOCM is currently one of the safest open-heart procedures with mortality risk <1% in experienced centers. Resolution of heart failure symptoms is evident with improvement by ≥1 NYHA functional class in >90% of patients with 75% becoming asymptomatic (i.e., from NYHA functional class III/IV to class I). In addition to improved quality of life, surgery reduces frequency of atrial arrhythmias and improves long-term survival to mirror that of the general population.
Cleveland Clinic has performed more than 3,000 myectomy procedures, with mortality 0.7% and <4.5% of patients requiring pacemakers. Due to the strong collaboration between Cleveland Clinic cardiac surgeons in both Ohio and Florida, this surgery is available to patients in Florida.
Dr. Smedira is Surgical Director of the Hypertrophic Cardiomyopathy Center at Cleveland Clinic's Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute in Cleveland, Ohio. Dr. Brozzi is Surgical Director of the Acute Mechanical Circulatory Support Program at Cleveland Clinic Weston Hospital.
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.