Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/37215b0f-5572-4aaf-89f1-2917eaac8db4/multimodality_cardiac_imaging_HVTI_FL)
Cardiac Imaging
By: David Lopez, MD, cardiologist and specialist in cardiovascular imaging in the Department of Cardiovascular Medicine at Cleveland Clinic Weston Hospital.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is reprinted from Cardiac Care: An Update for Physicians from the Heart, Vascular and Thoracic Institute (Spring 2024)
Many anatomical and functional abnormalities occur as a result of hypertrophic cardiomyopathy (HCM). Thick walls with disarray of muscle fibers and scar tissue are the primary substrates for common symptoms including shortness of breath, chest pain and palpitations or cardiac events including heart failure, syncope, and even sudden cardiac death (SCD).
Multimodality cardiac imaging is the foundation for characterizing, guiding management and determining prognosis of HCM. Most patients with HCM will have an echocardiogram, stress echocardiogram, and cardiac MRI (CMR) at presentation. These imaging studies are coupled with additional tests such as rhythm monitors, gene testing and, sometimes, cardiac catheterization to complete each patient’s evaluation.
CMR is best suited to distinguish mimics or phenocopies of HCM that include physiologic conditions like athlete’s heart and pathologic conditions like cardiac amyloidosis (CA) and Fabry disease (FD). This is an essential first step to verify a patient has HCM. The management of these conditions is vastly different.
Transthoracic echocardiography (TTE) is the first-line diagnostic test in the evaluation of HCM. TTE is not specific for the diagnosis of HCM but it helps exclude other structural abnormalities that cause increased left ventricular (LV) wall thickness, including a subaortic membrane and aortic valve stenosis. TTE findings typical of HCM include increased LV wall thickness, systolic anterior motion of the mitral valve, LV outflow tract obstruction (LVOTO), abnormal diastolic function and abnormal myocardial deformation or strain. CMR is usually performed following an abnormal TTE indicative of HCM.
Advertisement
A comprehensive multi-parametric CMR examination allows for confirmation of HCM, characterization of morphology and severity of hypertrophy, assessment of LV function, exclusion of phenocopies, and information for SCD risk stratification. The protocol must include imaging with gadolinium contrast media. CMR cine imaging improves detection of hypertrophied segments and allows accurate measurement of wall thickness.
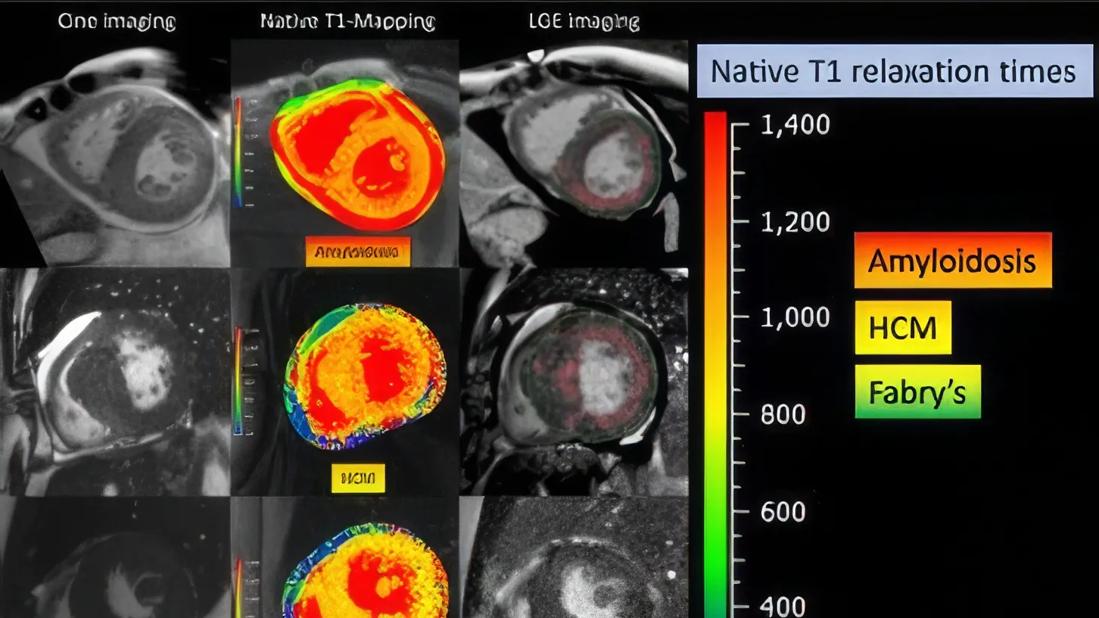
T1-mapping has emerged as a valuable tool for myocardial tissue characterization which helps differentiate HCM, CA and FD (Figure 1). Late gadolinium enhancement (LGE) imaging allows detection of interstitial fibrosis (Also Figure 1). CMR markers associated with increased risk of SCD that inform recommendation for a primary prevention implantable cardiac defibrillator (ICD) include myocardial wall thickness ≥ 30 mm, LV ejection fraction <50%, an apical aneurysm and/or LGE burden ≥15% of the left ventricular mass. Assessment of flow helps characterize location of LVOTO by differentiating flow acceleration due to SAM from non-HCM mechanisms.
Surveillance CMR is recommended every 3-5 years in those who initially do not meet criteria for primary prevention ICD but have potential to progress and may warrant ICD in the future. Figure 2 illustrates the progression of apical hypertrophy to apical aneurysm in a 10-year follow-up period. Surveillance ECG may provide clues that myocardial changes are taking place. Note the loss of QRS and T-wave voltage on ECG across the same monitoring period.
Advertisement
A crucial step in the characterization and management of HCM is to establish the presence or absence of LVOTO, which is not always seen on examinations at rest. Exercise stress echocardiography (SE) is performed to show presence of provokable LVOTO, assess hemodynamic response to exercise and objectively define a person’s exercise capacity. In individuals with obstructive HCM, SE guides treatment recommendations and allows monitoring of therapeutic effects.
Other imaging modalities may be used when echocardiography or CMR do not provide the necessary information or there is a contraindication. Cardiac computer tomography (CT) can define cardiac anatomy (including detecting a myocardial bridge often present with HCM) but provides limited myocardial tissue characterization. Coronary CT angiography is often used in preoperative planning of young HCM patients undergoing surgical septal reduction therapy. Transesophageal echocardiography is utilized intraoperatively to guide septal myectomy.
Otherwise, it is occasionally also used when there are unresolved concerns for alternative mechanisms of LVOTO or to better characterize the mechanism of mitral regurgitation.
The road to HCM diagnosis and treatment is often tortuous, even among experienced clinicians. Appropriate use of multimodality cardiac imaging helps to promptly and safely arrive at the correct diagnosis in order to provide the indicated treatment for those with suspected HCM. At Cleveland Clinic Weston Hospital, our HCM physicians and imaging specialists work closely together as a multidisciplinary team to care for high volumes of HCM patients and have expertise in all of these important imaging modalities.
Advertisement
Dr. Lopez is a clinical cardiologist and specialist in cardiovascular imaging in the Department of Cardiovascular Medicine at Cleveland Clinic Weston Hospital.
Advertisement
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.