Impact on tumor immune microenvironment and response to immunotherapy
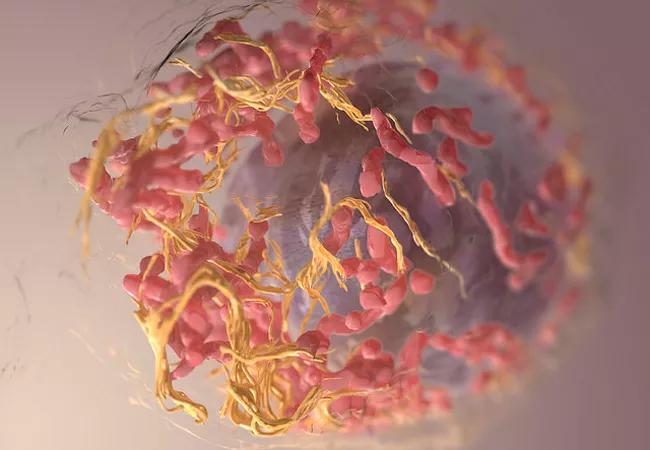
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56cece70-779f-471b-a2e6-cd0cb37862e5/20496714399_9d12e253e1_z_650x450_jpg)
20496714399_9d12e253e1_z_650x450
Advanced melanoma is the prototype tumor for immune and genomic-targeted therapy. Immunotherapy is potentially curative, however the majority of patients do not respond. Immunotherapy non-responsiveness has been attributed to a reliance upon preexisting tumor immune recognition [“immune-inflamed” tumor microenvironment (TME)] in order for this therapy to work. The determinants of this pre-existing immune recognition are not known, but recognition loosely associates with overall tumor mutational burden (TMB).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jennifer Ko, MD, PhD, dermatopathologist, and Medical Director of the Central Biorepository in the Pathology and Laboratory Medicine Institute, hypothesized in her recent research that certain molecular driver mutations may render a melanoma tumor more or less immunogenic, and hence determine its responsiveness to immunotherapy. To begin to answer this question, Dr. Ko worked with Ying Ni, PhD, in the Center for Clinical Genomics, and Sophia Jia in Quantitative Health Sciences, to examine somatic DNA mutation and RNA expression data for cutaneous melanoma from the public database The Cancer Genome Atlas (TCGA).
They studied tumor mutational burden, specific driver mutations, immune related RNA expression data and various clinicopathologic features from 479 tumors to investigate the correlations among multi-omics with clinical characteristics and outcomes.
Preliminary evidence shows that the “immune-inflamed” TME predicted improved survival (P < 0.001) whereas mitotic rate and Ki67 expression predicted worse survival (P = 0.004 and P = 0.003 respectively).The tumor mutational burden did not correlate with survival (P = 0.39), yet was positively associated with the number of hot-spot mutations and the number of genes mutated in the driver mutation panel utilized (P < 0.001). The correlation between TMB and a pre-existing inflamed microenvironment was not statistically significant (P = 0.07). Specific driver mutations within the panel were found to correlate with an inflamed TME.
Advertisement
Overall, the findings suggest that the driver mutational signature in melanoma influences both the tumor immune microenvironment and responsiveness to immunotherapy. Ongoing studies are validating these findings in a cohort of Cleveland Clinic patients.
To learn more about the immunology of melanoma, read Dr. Ko’s review in Clinics in Laboratory Medicine.
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting