First agent in a new class of noncytotoxic cancer drugs
At the 2018 American Society of Hematology annual, investigators from Cleveland Clinic Cancer Center presented data demonstrating efficacy of a first-in-class inhibitor (ED2-AD101) of SMARCA5/CHD4 (SWI/SNF-related matrix-associated actin-dependent regulator of chromatin subfamily A member 5/chromodomain helicase DNA binding protein 4) in cell-based assays of acute myeloid leukemia (AML).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is the first agent from a new class of drugs that exerts its effect not through direct cell death but through terminal differentiation of AML cells, turning them into nondividing granulocytes,” says Yogen Saunthararajah, MD, hematologic oncologist at Cleveland Clinic. “We discovered this scaffold by screening a small molecule library of compounds that induce terminal differentiation of leukemia cells. We then executed a gamut of assays to identify the specific molecular targets of this family of potent differentiation-inducing compounds.”
Dr. Saunthararajah explains that in drug discovery, it is important to not only think about the molecular target, but also to consider the downstream pathway by which the drug is proposed to act on diseased cells.
“It is important to think about the pathway because if a pathway downstream of the target is inactivated in cancer cells, then the cancer cells readily resist multiple different drugs that depend on that same pathway,” he explains. “For example, most of our drugs to treat leukemias and other cancers use apoptosis as their pathway of action. But most leukemias and cancers attenuate or inactivate the apoptosis program, conferring resistance to multiple drugs and radiation. Meanwhile, normal dividing cells, with intact apoptosis programs, are destroyed.”
He adds that this new drug class is significant because it does not stop the proliferation of AML cells by apoptosis; rather, it utilizes a different mechanism of action. Because hundreds of monocyte and granulocyte terminal-differentiation genes are epigenetically suppressed in AML cells, they can escape terminal granulomonocytic fates.
Advertisement
“The important aspect is that these proliferation-termination genes are physically intact and poised for activation by the master transcription factors that are highly expressed in AML cells,” says Dr. Saunthararajah. “This new class of drugs exploits this biology of AML to terminate the proliferation of malignant cells without harming normal, dividing hematopoietic cells.”
In their search for new drug candidates, Dr. Saunthararajah and colleagues specifically excluded those molecules that cause apoptosis and focused on compounds that only cause differentiation of leukemia cells. The ED2-AD101 class of compounds that they identified causes selective differentiation of leukemia cells by inhibiting a class of epigenetic enzymes called the ISWI (Imitation SWItch) family — members of this enzyme family include SMARCA5 and CHD4.
At concentrations ranging from less than 1 to 10 mM, ED2-AD101 effectively suppressed the growth of AML cells containing a spectrum of genetic alterations, including genetic inactivation of apoptosis. AML cell proliferation was terminated by activation of the terminal granulocytic differentiation program. The growth of normal, healthy hematopoietic cells was spared.
Dr. Saunthararajah cautions that there is still much work to do before these molecules can be used in the clinic.
“We are continuing to work on refining the molecules and have to conduct extensive, preclinical in vivo proof-of-principle experiments using patient-derived xenotransplant models of leukemia,” he says. “We are optimistic, however, that these molecular scaffolds hold within them the promise for an alternative, rational, effective and nontoxic paradigm of leukemia and cancer therapy.”
Advertisement
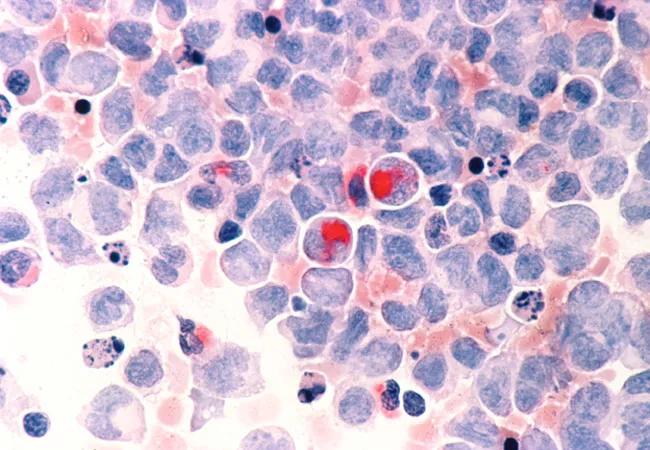
Image: Human cells with acute myelocytic leukemia (AML) in the pericardial fluid, shown with an esterase stain at 400x. Source: NCI Visuals Online.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors