Retrospective analysis finds no evidence of benefit, but more study needed
Intraoperative multimodal (IOM) monitoring, which provides real-time feedback on spinal cord integrity, did not lead to better outcomes in patients undergoing a pedicle subtraction osteotomy (PSO) of the lumbar spine during a decade’s experience involving 101 patients at Cleveland Clinic. So concludes a retrospective study presented at the American Association of Neurological Surgeons (AANS) 2019 annual scientific meeting this week.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Monitoring uses a lot of resources and sometimes leads to false-positive findings, so it’s important to evaluate whether it’s useful,” says senior author Michael Steinmetz, MD, Chair of Neurosurgery at Cleveland Clinic. “Although we didn’t detect benefits from IOM monitoring during PSOs of the lumbar spine, we must still consider whether there’s a very small chance that it prevents a life-changing injury, which would make monitoring worthwhile.”
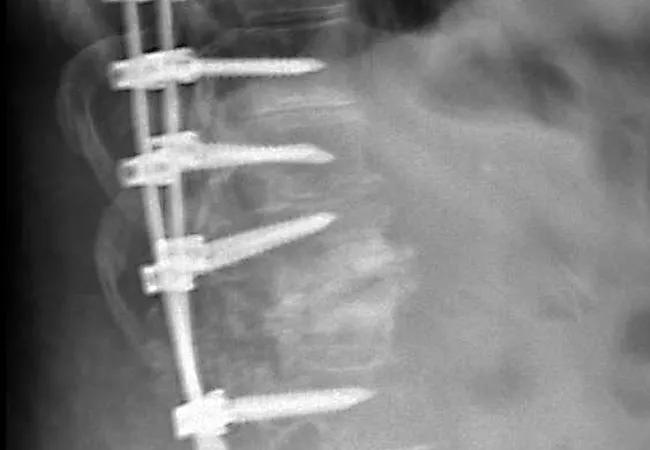
IOM monitoring — which most commonly uses motor and somatosensory evoked potentials and spontaneous (free-running) electromyography — has largely become standard practice for PSOs of the thoracic spine. It is used in an effort to minimize accidental neurological injury to the spinal cord, nerve roots and associated structures. Iatrogenic injury from surgery to correct a spine deformity can range from minor sensory disturbances to complete paralysis.
But while benefits of IOM monitoring for PSOs on the thoracic spine have been documented in other studies, its usefulness is less certain for PSOs of the lumbar spine, where the spinal cord typically extends only to the level of the first or second lumbar vertebra. Accordingly, guidelines for its use in this setting have not been established. As a result, whether IOM monitoring is used during a PSO of the lumbar spine is largely a matter of surgeon preference.
In a recent narrative literature review (Clin Spine Surg. 2018 Nov 6 [Epub ahead of print]) of IOM monitoring for PSOs of the lumbar spine, a team of Cleveland Clinic authors led by Dr. Steinmetz concluded that more research is needed to establish the risks and benefits and to set guidelines for IOM monitoring in this setting.
Advertisement
For the study presented at the AANS meeting, a retrospective chart review was conducted of adult patients at Cleveland Clinic who underwent a lumbar PSO from 2007 to 2017. A total of 101 patients were included in the analysis, with the procedures being performed with or without IOM guidance according to surgeon preference.
Patients were evaluated with the self-reported 39-item Parkinson’s Disease Questionnaire (PDQ-39) at baseline and at three months after surgery. Patients who did and did not receive IOM monitoring during their operation were compared in terms of PDQ-39 quality-of-life (QOL) scores and also in terms of the proportions who achieved a minimal clinically important difference (MCID) in PDQ-39 score, defined as an increase of 4.72 points, from baseline to three-month follow-up. Multivariate analysis was used.
No statistically significant differences were found between patients who did and did not receive IOM monitoring in QOL scores (P = 0.230) or in MCID achievement at three months (P = 0.196). Factors that did have a statistically significant impact on rates of achieving MCID were younger age and female sex.
Dr. Steinmetz notes that IOM monitoring is progressively becoming the standard of care in surgeries for spinal deformity for good reason: Its utility for preventing nerve and cord injury during thoracic surgery has been established.
He says the jury is still out on whether it is worthwhile for surgeries of the lumbar spine, although this study’s findings could increase the level of confidence for surgeons who choose not to monitor during these types of operations.
Advertisement
Dr. Steinmetz’s research group is currently planning a large, prospective multicenter study to help resolve these unknowns and advance toward establishing practice guidelines.
“While it is possible that IOM monitoring is not needed for PSOs of the lumbar spine, there may be specific circumstances in which it is useful, or certain types of monitoring may be more helpful than others,” he adds. “A large data set can help us determine these nuances and make evidence-based recommendations.”
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits