Study finds high coverage denial for women, patients with prior oral appliance use
Two subgroups of patients with obstructive sleep apnea (OSA) — women and those who have previously used oral appliances to manage OSA — are less likely to receive approval for insurance coverage of upper airway stimulation (UAS) treatment, whereas other groups — men, patients who have had previous OSA surgeries and patients who have used positive airway pressure (PAP) devices — are more likely to gain insurance coverage. So finds a prospective study published in the Annals of the American Thoracic Society.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We undertook this multicenter study to understand what happens to patients with OSA who are not approved for UAS, which is an alternative to PAP for patients who don’t tolerate or aren’t adherent to PAP therapy,” says lead author Reena Mehra, MD, MS, Research Director of Cleveland Clinic’s Sleep Disorders Center. “These individuals have very limited options for treatment. Therefore, it is important to understand if there are certain subgroups who are vulnerable to insurance coverage denial, especially since coverage for UAS has been inconsistent and somewhat arbitrary compared with insurance approval for PAP and airway surgery.”
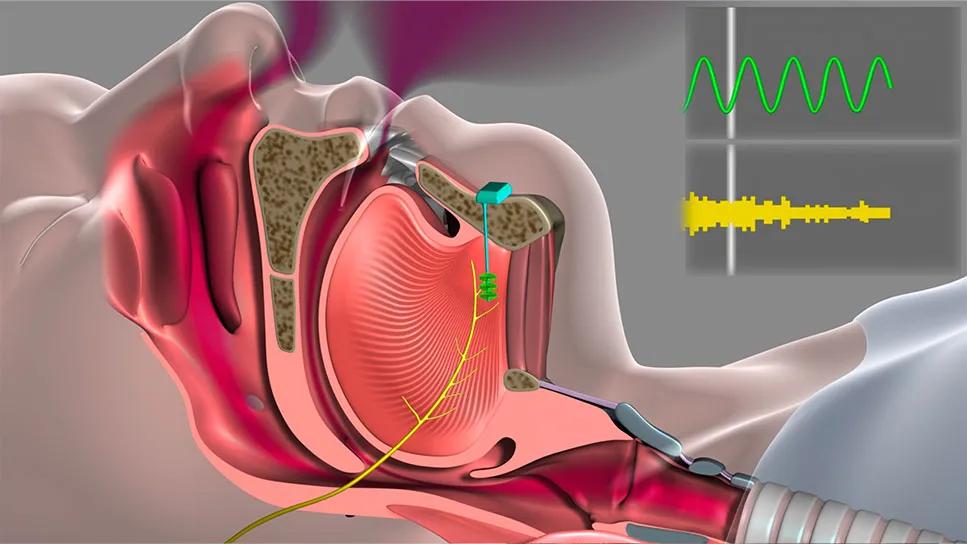
UAS entails surgical implantation of a cuff electrode to stimulate the hypoglossal nerve, which prompts the tongue to move forward in the mouth, thus opening the airway. A programmable neurostimulator and a pressure-sensing lead that detects respiration are also implanted. Multiple studies have demonstrated that UAS significantly reduces OSA burden and patient symptoms with a high degree of adherence to the nightly therapy. “It is recognized that adherence with UAS is higher than with PAP therapy,” Dr. Mehra notes.
The parallel-arm multicenter cohort study enrolled 350 individuals with health insurance and PAP intolerance who qualified for UAS implantation. Its goal was to compare OSA burden between patients who did and did not receive insurance coverage approval for UAS.
Significantly greater reductions in the apnea-hypopnea index were found in patients who underwent UAS (median follow-up, 12 months) compared with those who did not due to insurance denial (median follow-up, 6 months). UAS-treated patients also reported significantly greater improvements in subjective measures of dozing propensity and overall sleep-related outcomes.
Advertisement
“When we analyzed factors related to insurance approval, we were surprised to find that women and those who had used oral devices had a higher percentage of insurance denials, the reasons for which are unclear,” Dr. Mehra observes.
She notes that there may be an underlying perception in the insurance industry that OSA is more common in men than in women and thus UAS is less necessary in women. In addition, there are some data indicating that women appear to be denied medical care reimbursement in general more often than men are. “Although there is not much literature on sex-specific differences in insurance approvals for treatments of other disorders, denials for other medical devices, such as cardiac defibrillators, are not uncommon for women,” she says. Similarly, a 2018 study of 30,000 patients in the general U.S. population showed that women were more likely than men to be denied reimbursement for visits to the emergency department.
The denials associated with previous use of oral appliances were even more perplexing, says Dr. Mehra. She speculates that because these appliances are a surrogate for the degree of OSA severity, insurers may believe that people for whom oral appliances are attempted generally have a milder or moderate degree of OSA. Alternately, these individuals may be perceived by insurers to have certain anatomical features that make them less than ideal candidates for UAS.
“We need to investigate further to understand the reasons behind these denials and whether they are valid or unjustified,” she says. “Our previous research analyzing data from the international ADHERE registry showed that women respond better to UAS than men do. This finding, when combined with our new findings, suggests that insurance denials may be preventing us from treating many of the patients who are most likely to benefit. These data can be used to lobby insurance companies to cover patients who are being left without treatment alternatives — and to influence health policy to focus on the most vulnerable patients.”
Advertisement
Dr. Mehra’s research team is continuing to investigate the potential benefits of UAS. “We are highly interested in the relationship between cardiovascular health and sleep apnea,” she notes. “We are also interested in how PAP versus UAS affects blood pressure — work being led by my Sleep Disorders Center colleague Harneet Walia, MD — and the mechanical functioning of the heart.”
Dr. Walia is also leading additional Cleveland Clinic research efforts to compare the efficacy of home testing versus in-lab testing for post-treatment monitoring of patients who have undergone UAS.
“The more information we have on UAS, both medical and insurance-related, the better we can apply this technology to effectively manage our patients with OSA,” Dr. Mehra concludes.
Advertisement
Advertisement

Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains