A recent clinical trial tested neoadjuvant therapies
Neoadjuvant drug therapy can produce a pathologic complete response (pCR) in breast cancer patients, but success varies depends on the type of breast cancer present. Investigators are refining treatments in the hopes of reducing this variability.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
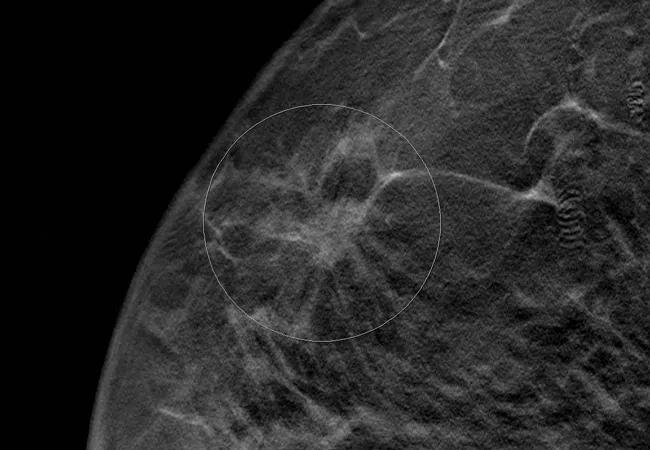
During a recent clinical trial, the results of which were published in the Journal of Clinical Oncology, researchers gave women with estrogen-receptor (ER) positive breast cancer endocrine therapy preoperatively. After two weeks, the enrollees underwent a biopsy, and based on the level of Ki67 protein in that test, either continued to receive endocrine therapy or were switched to chemotherapy.
The use of Ki67 level turned out to be a good predictor of who might do well on endocrine therapy alone, but it was not as effective for predicting those who might do well on chemotherapy, if the endocrine therapy failed.
“In some patients treatment with endocrine therapy alone is sufficient and gives a good outcome, and this study helped define such a group of patients,” says G. Thomas Budd, MD, staff physician in Cleveland Clinic Cancer Center and one of the authors on the paper. “What this study was not so good at, however, was predicting who responds to chemotherapy.”
The study enrolled 245 postmenopausal women with clinical stage II or III ER–positive breast cancer. The women were randomly assigned to 16 to 18 weeks of neoadjuvant endocrine therapy which consisted of one of three aromatase inhibitors (AI): exemestane 25 mg once daily, letrozole 2.5 mg once daily or anastrozole 1 mg once daily.
After two weeks of endocrine therapy, all the patients had a breast biopsy. Of the 245 enrollees, 165 (69.9 percent) had a Ki67 value of less than 10 percent, while 49 (20.8 percent) had a Ki67 value of greater than 10 percent. Twenty-two (9.3 percent) had insufficient tumor to make a Ki67 determination.
Advertisement
Most of the women with a low Ki67 value responded well to endocrine therapy and had low relapse rates. After 5.5 years of median follow-up, for instance, only four of the 109 patients with a Preoperative Endocrine Prognostic Index (PEPI) score equal to zero relapsed. PEPI is a tool based on factors such as tumor size, nodal status and Ki67 levels that can predict reoccurrence of breast cancer.
The majority of women with a Ki67 value of greater than 10 percent and who were switched to chemotherapy, however, did not respond well to either treatment.
“I think this study indicates that there are a group of patients who need treatment in addition to endocrine therapy and are not that responsive to chemotherapy and may need alternative approaches,” says Dr. Budd. “Future studies will need to look at the role of those alternative approaches.
Dr. Budd says the study was surprising because investigators hypothesized that 20 percent of patients with Ki67 values of greater than 10 percent would respond to chemotherapy and achieve pCR, but the data showed only 5. 5 percent of that group responded.
He says another neoadjuvant trial, which is ongoing, is experimenting with adding fulvestrant, a selective ER degrader, to endocrine therapy, while an upcoming study will examine the role of CDK4/6 in the neoadjuvant setting.
“There may be other agents that can be investigated in those patients who require more than simple endocrine inhibitors,” Dr. Budd says. “There are new approaches, other than chemotherapy, that seem to augment the effectiveness of endocrine treatment.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors