Advertisement
A case study of this rare presentation
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 29-year-old woman presented to the emergency room with symptoms of abdominal pain and vaginal bleeding. Ultrasound confirmed a 9+5 week pregnancy located within the lower uterine segment with crown lump length measuring 22mm, which extended into a previous cesarean section scar. The lower uterine segment was ballooned anteriorly abutting the bladder without an obvious plane. She had six previous pregnancies, including four previous cesarean section deliveries, and a strong desire for uterine preservation. Other relevant medical history included tricuspid valve replacement in 2016. Physical exam revealed a 10-week uterus, mildly tender to palpation, and speculum examination revealed a closed cervix with scant red brown blood. Her blood pressure and pulse were within normal limits; her HCG was 53,654 mIU/ML.
A definitive diagnosis of cesarean scar ectopic pregnancy (CSEP) was made and the patient was admitted for uterine artery embolization and ultrasound guided intra-gestational sac methotrexate injection to decrease the blood flow to the ectopic pregnancy. She was followed with serial ultrasounds and beta HCGs, which trended down to 58.6 mIU/ML. She was ultimately scheduled for laparoscopic resection of the CSEP, isthmocele resection and repair, and lysis of adhesions.
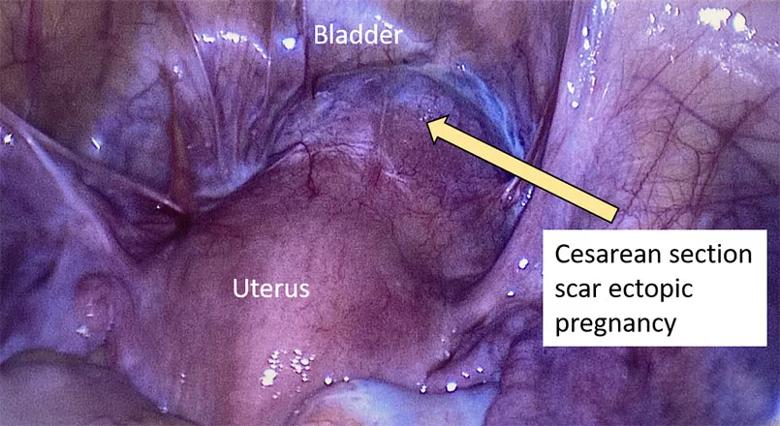
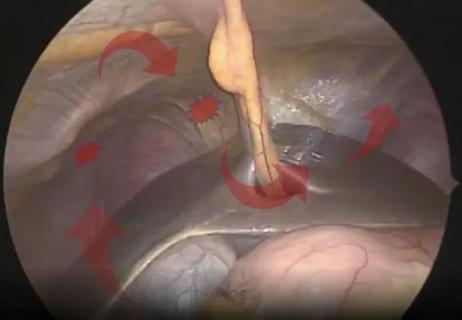
Laparoscopic image revealing a cesarean section scar ectopic pregnancy at 9+5 weeks gestation.
To help with hemostasis, a dilute vasopressin solution was injected transvaginally into the cervical stroma as well as laparoscopically around the isthmocele. We noted that the gestational sac contained a fetus at 9 weeks. We excised the remaining isthmocele, inserted a RUMI manipulator and performed a gentle curettage through suprapubic port to ensure all products of conception were removed. We then closed the myometrium. After ensuring water-tight closure, we placed the isthmocele tissue in an endocatch bag and removed it through the umbilicus without difficulty.
We extubated the patient and transferred her to the PACU in stable condition. The patient was discharged home the same day.
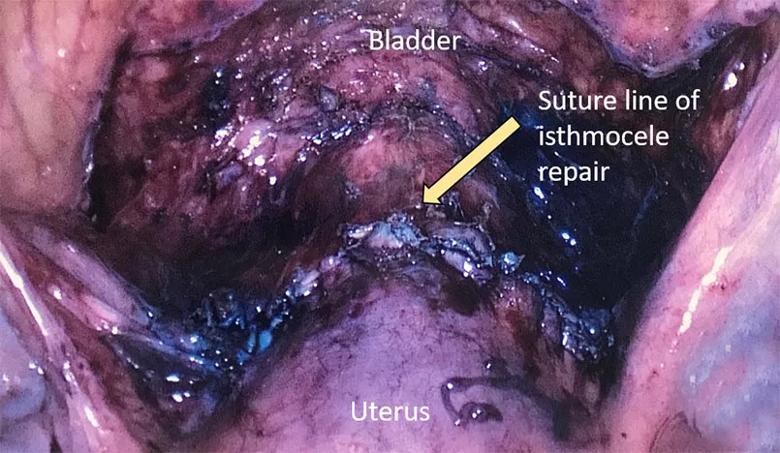
Laparoscopic image status post laparoscopic removal of cesarean section scar ectopic pregnancy and isthmocele repair.
Advertisement
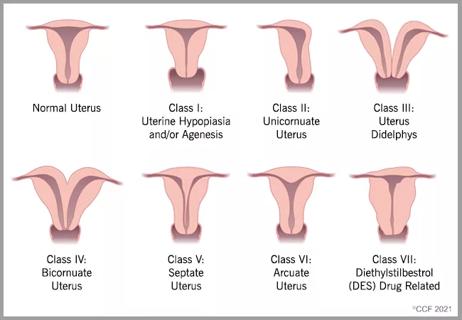
CSEP — defined as the implantation of a blastocyst within a previous cesarean scar — is rare, occurring in approximately 1 in 2,000 pregnancies. CSEP accounts for only about 6% of all ectopic pregnancies in patients who have had previous cesarean sections. Before implanting, it is thought that the embryo may migrate through a defect in the lower uterine segment or a microscopic fistula in the scar. Patients may present with abdominal cramps, low abdominal pain or vaginal bleeding, or they may be asymptomatic and present for evaluation for ectopic pregnancy. If undetected, CSEP can lead to uterine rupture or hemorrhage. Diagnosis is made via ultrasound, and often requires a high index of suspicion. Medical treatment may take months and carries the risk of uterine rupture and life-threatening hemorrhage. Laparoscopic resection, in this particular case, removed the products of conception and allowed for repair of the defect with uterine preservation.
Advertisement
Advertisement

Surgical video highlights techniques for optimizing myomectomy

Study indicates patients can have confidence about potential outcomes

Laparoscopic surgery provides relief for teenage patient with adenomyoma and endometriosis

A large nodule had strangulated the patient’s ureter and invaded the vagina, bladder and rectum

Case study: Concomitant robot-assisted surgery without repositioning the patient
Analysis compares ovary removal to surveillance in asymptomatic patients
Cleveland Clinic delivers team approach to diagnosis and treatment of rare condition
Tips and techniques to help optimize resection and ablation of lesions in the diaphragm