Odds of seizure freedom diminish with each additional operation
Long-term seizure control is achievable in patients with failed prior epilepsy surgery, but the likelihood of success decreases with each reoperative attempt, regardless of other clinical factors. So finds the first single-center study of longitudinal outcomes and outcome predictors following epilepsy reoperations in a large cohort of patients with medically refractory focal epilepsy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, published by Cleveland Clinic Epilepsy Center staff in Epilepsia, proposes a novel concept of “surgical refractoriness” as a possible contributor to the diminishing returns from repeated epilepsy surgeries.
“Our findings, particularly the notion of surgical refractoriness of the epileptogenic zone, underscore the need for prudent selection of candidates for reoperative epilepsy surgery,” says the study’s corresponding author, Lara Jehi, MD, Research Director in Cleveland Clinic’s Epilepsy Center. “As our tools for seizure localization improve, there is an understandable urge to consider further surgery after a previous surgical failure, to address any residual epileptogenic tissue. However, our results build on other recent data suggesting that inherent and potentially genetic patient characteristics may raise the risk of operative failure regardless of the quality of localization and resection.”
Data on long-term outcomes and outcome predictors following repeat epilepsy surgery have been limited, with no published reports addressing outcomes after more than a single reoperation.
To fill the void, the authors reviewed clinico-radiologic characteristics of all patients who had surgery for intractable focal epilepsy at Cleveland Clinic from 1995 through 2016. For inclusion in the analysis, patients had to have at least one year of postsurgical follow-up data. For patients undergoing reoperation, the latest resection was deemed the index surgery.
The researchers analyzed both longitudinal seizure outcomes and predictors of those outcomes, first using univariate analyses and then multivariate Cox proportional hazard modeling. Primary outcomes of interest were postsurgical freedom from any seizure recurrence and probability of achieving an Engel score of I, which indicates eventual favorable seizure outcome (allowing for some early postoperative seizures) or seizures only during physiological stress (e.g., drug withdrawal).
Advertisement
Of the 898 patients who met inclusion criteria, one-third were pediatric patients and 68% underwent temporal lobe resection. Mean follow-up was 4.2 years.
Among the 898 study subjects, 110 (12.2%) had reoperations — 92 cases in which there was one resection prior to the index surgery and 18 cases with two or more prior resections.
At two years after index surgery, an Engel score of I was achieved by 69% of the cohort with no prior epilepsy surgeries compared with only about 40% of those with one or more prior surgeries (P < 0.001). Rates of complete seizure freedom at two years were 58% for those with no prior surgeries, 49% for those with one prior surgery (P = 0.003) and 39% for those with two or more prior surgeries (P = 0.028).
On multivariate analysis, three factors were found to be predictive of postsurgical seizure recurrence:
“Prior literature to guide selection of patients for repeat epilepsy surgery has been extremely limited, and no previous studies have explored the effect of multiple reoperations,” says Dr. Jehi. “We have shown that even though a substantial share of patients can become seizure-free following repeat epilepsy surgery, the chances of achieving seizure freedom or a good Engel score diminish with each additional surgery.”
The researchers note that the association between number of surgeries and worse seizure outcomes withstood multivariate analysis even when all traditional outcome predictors and surrogates of poor seizure localization were controlled for. “This association seemed to correlate more closely with patients’ inherent biological characteristics, such as sex and predisposition to secondary generalization, than with poorly localized epilepsy,” says Cleveland Clinic neurosurgeon William Bingaman, MD, a study co-author. “This suggests that at least some patients whose seizures don’t respond to multiple operations may have what we’ve called ‘surgical refractoriness.’”
Advertisement
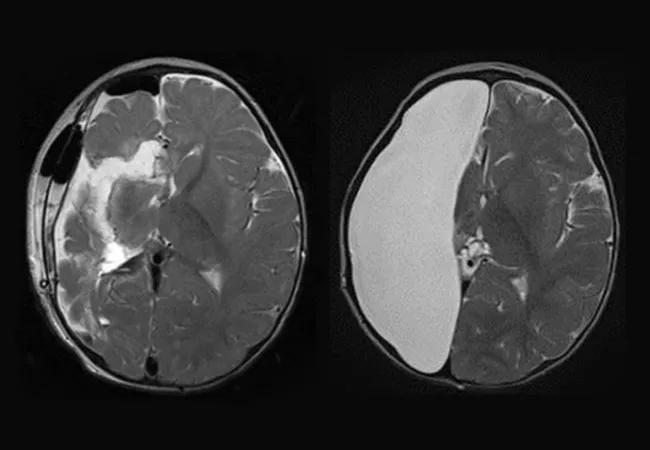
The authors describe this concept as “a widespread, ‘malignant’ epileptogenic network with a tendency to develop new epileptogenic zones upon resection of the prior zone, causing a progressive disease state.” While they emphasize that further research is needed to confirm and delineate the notion of surgical refractoriness, the authors contend that better understanding of this patient profile may help identify patients who are not good surgical candidates — at least not for repeat surgery.
“Our findings emphasize the need for prudence in evaluating candidates for reoperation,” observes Dr. Jehi. She notes that the characteristics found to significantly predict seizure recurrence on univariate analysis were male sex, secondary generalization, higher preoperative seizure frequency, epileptogenic focus in the dominant hemisphere, need for an invasive evaluation and early seizure recurrence after prior surgery. “The presence of these factors should give patients and clinicians pause before considering repeat epilepsy surgery,” she says.
“These findings also highlight the importance of conducting more research into the genetic mechanisms of epilepsy and of seizure outcomes after epilepsy surgery,” Dr. Jehi concludes.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help