Pioneering and refining the approach in pyeloplasty, nephrectomy and more
Low anterior access (LAA) can further enhance the benefits of single-port (SP) robotic approaches in certain urologic surgeries, including pyeloplasty, partial nephrectomy and ureteric reimplant, according to multiple reports and extensive experience at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The single-port robotic system allowed us to further regionalize surgeries and avoid the intraperitoneal space,” says Jihad Kaouk, MD, Director of the Center of Advanced Robotic and Image-Guided Surgery at the Glickman Urological & Kidney Institute. “With the addition of low anterior access, we can spare upper abdominal muscles, improve cosmesis and decrease postoperative pain, creating a better perioperative and postoperative experience for our patients.”
According to Dr. Kaouk, the SP robotic system allows for the most minimally invasive surgery available to date by simultaneously introducing three multijointed, wristed surgical instruments; a steerable 3D high-definition camera; and an assistant accessory port into the abdomen through one small incision. The single arm allows 360-degree multiquadrant access. This design provides improved maneuverability through limited surgical fields and permits new and different surgical routes that have not been feasible before.
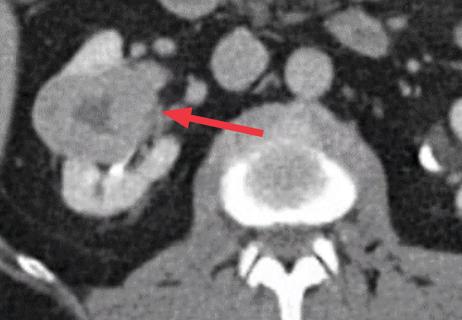
The SP system makes possible a more streamlined surgical technique for urologic procedures, such as with direct percutaneous access into the bladder for transvesical prostatectomy (opioid-sparing outpatient radical prostatectomy) and direct access into the retroperitoneum for various upper tract procedures. This allows for the complete preservation of the peritoneum and all intraperitoneal organs. In a retroperitoneal approach, surgeons can perform partial nephrectomies for tumors located on the anterior surface of the kidney and are not limited to posteriorly located tumors, as is the case with standard retroperitoneal robotic partial nephrectomies.
Advertisement
Under the direction of Dr. Kaouk, Cleveland Clinic was the first to report using LAA with the SP robot for pyeloplasty and retroperitoneal partial nephrectomy. A report from the 20th meeting of the European Urology Association demonstrated that the technique enables opioid-sparing recovery and discharge within 24 hours for anterior, posterior and lateral tumors.
“The SP robotic system solves the problem of the working distance from an inferior incision to the kidney, even when working in the upper pole,” says Dr. Kaouk.
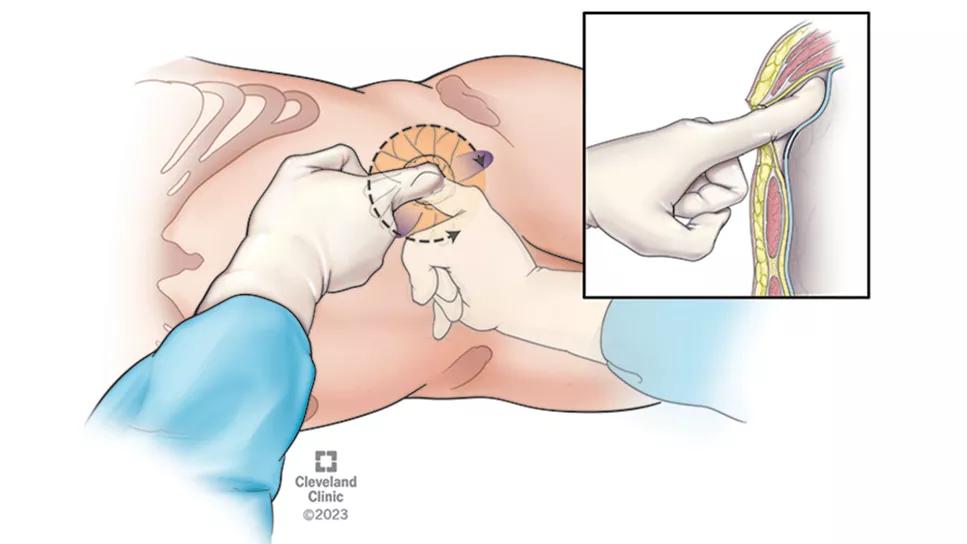
LAA access involves a single 3 cm incision two fingers’ breadth above the superior pubic ramus. Then, the surgeon performs blunt finger dissection to open the extraperitoneal space for the insertion of the purpose-built SP access kit.
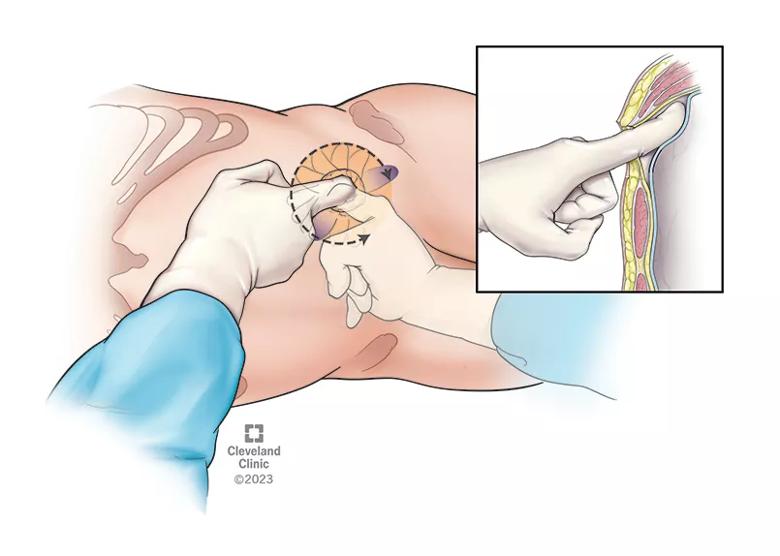
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd7bee8e-10ab-496a-b653-170f860c5b64/low-anterolateral-access2)
The surgeon preserves the peritoneum by gently pushing it down before inserting the kit. The SP robot is then docked at an acute angle towards the ipsilateral kidney, with the camera either at 6 or 12 o’clock depending on the location of the tumor.
The video below shows the full technique through specimen retrieval.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_6w6l2crx/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
“Our carefully selected patients love this approach,” notes Dr. Kaouk, “because recovery is faster and less painful, and cosmesis is improved. It has also allowed us to expand our indications for single-port surgery as we can reach more tumors retroperitoneally, even those located on the anterior surface of the kidney.”
Advertisement
Advertisement
AUA guideline offers specific criteria for deciding between partial versus radical nephrectomy

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Milestone minimally invasive surgeries reduce pain and recovery time

Enhanced visualization and dexterity enable safer, more precise procedures and lead to better patient outcomes

Least-invasive open-heart AVR option to date yielded rapid recovery in all cases

Cleveland Clinic is among the first in the U.S. to perform the procedure

Minimally invasive pancreas-kidney replacement reduces patient’s pain, expedites recovery

First single-port renal vein transposition reduces recovery time and improves outcomes