Minimally invasive pancreas-kidney replacement reduces patient’s pain, expedites recovery
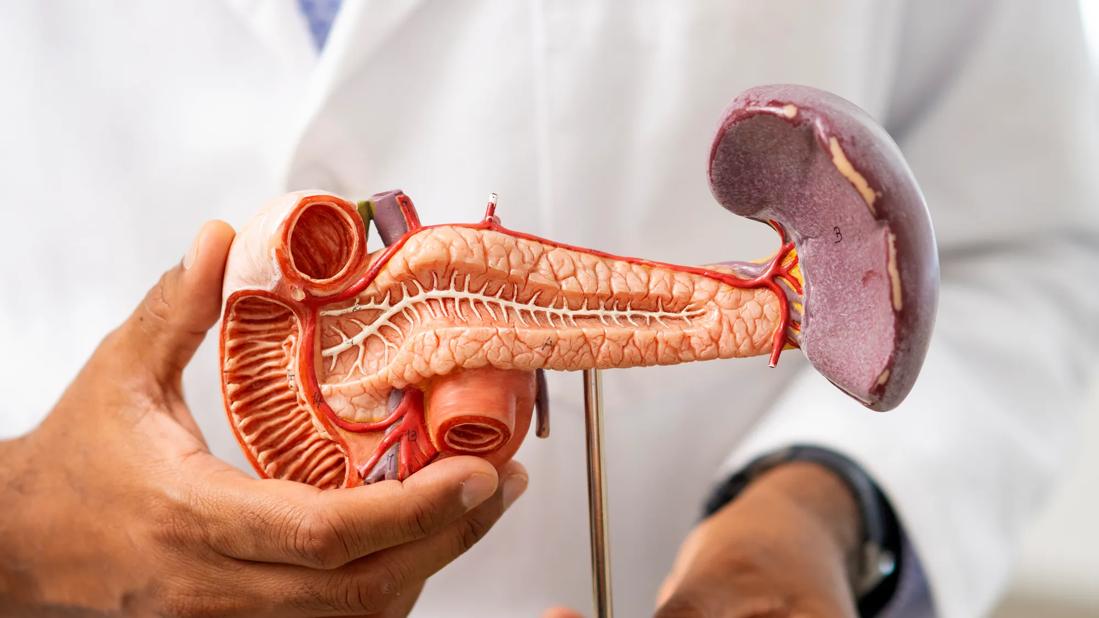
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/11a3ebfe-8048-4ef0-922f-fb8664e2f09a/CNR_5115479_08-20-24_098_DG)
3-D medical pancreas
A Cleveland Clinic surgical team has performed the institution’s first robot-assisted simultaneous pancreas-kidney transplant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The complex minimally invasive dual-organ procedure, which only a few medical centers in the world have undertaken, resolved the patient’s renal failure and restored insulin independence while decreasing pain, opioid reliance and recovery time. It builds on the expertise of Cleveland Clinic’s robot-assisted kidney transplant program.
The patient “is doing really well,” Alvin Wee, MD, Surgical Director of Renal Transplantation, says of the 41-year-old transplant recipient, who was operated on in January 2025. “Her diabetes is controlled and she is no longer on dialysis. When you see a patient dramatically improve virtually overnight, it makes our team feel very gratified.”
Chronic pancreatic dysfunction due to inflammation or disease impairs insulin production and leads to diabetes. Poorly controlled diabetes and chronic hyperglycemia, in turn, damage renal vasculature (among other pathologies), resulting in diabetic nephropathy.
Diabetes is the leading cause of chronic and end-stage kidney disease globally, accounting for approximately half of all cases. Both diabetes and end-stage renal failure shorten patients’ lifespans and significantly reduce quality of life.
Since the first successful operation in 1966, pancreas-kidney transplantation, performed either simultaneously or sequentially, has been used to treat uremia and achieve insulin independence in patients with type 1 diabetes and nephropathy.
Pancreas-kidney transplantation traditionally has necessitated an open surgical approach involving an extensive midline abdominal incision.
Advertisement
Such large midline incisions are associated with substantial postoperative pain and concomitant analgesia requirements, protracted recovery time, cosmetic issues, and an increased risk of postsurgical complications such as improper wound healing and incisional hernias.
Wound complications are a heightened concern in diabetic patients who are transplant candidates, especially those with obesity.
Minimally invasive surgical techniques have been developed to address issues of pain, analgesia, recovery time and wound healing, with applicability in transplant surgeries.
Minimally invasive laparoscopic kidney transplantation was first performed by a Spanish surgical team in 2009. The technique has not been widely utilized, however. This is likely because, among other things, laparoscopic imaging of the surgical site is restricted to two-dimensional views and the range of motion of laparoscopic instruments is limited, making vascular anastomoses challenging.
The advent of remotely operated robotic surgical platforms beginning in the 1990s has greatly enhanced the field of minimally invasive surgery, including in transplantation. Robotic systems’ articulated arms and wristed instrumentation improve dexterity, enabling precise dissection and microsuturing in restricted spaces. Three-dimensional cameras and magnification provide better visualization. Motion tracking, movement scaling and damping and, most recently, haptic feedback, increase accuracy and reduce tremor.
French surgeons performed the first robot-assisted kidney transplant in 2001. Subsequent reports demonstrated that the robotic procedure’s patient and graft survival outcomes were comparable to those achieved with the open approach.
Advertisement
In 2012 an Italian surgical team reported performing the first robot-assisted pancreas transplant, sequential kidney-pancreas transplant and simultaneous pancreas-kidney transplant. Although the three procedures were successful, the simultaneous robot-assisted pancreas-kidney transplant took eight hours, considerably longer than an open approach.
The surgeons warned that long anastomotic times and extended warm ischemia could damage the pancreas graft and cautioned about the potential for postperfusion bleeding and unanticipated technical difficulties. They stressed the importance of extensive prior experience in conventional open kidney and pancreas transplantation as well as various types of abdominal robot-assisted operations before attempting the simultaneous robot-assisted pancreas-kidney procedure.
While the adoption of robot-assisted kidney transplantation and, to a lesser extent, robot-assisted pancreas transplantation, has gained traction, robot-assisted simultaneous pancreas-kidney transplantation remains limited to a very few highly specialized centers.
Undertaking the surgery was a natural progression for Cleveland Clinic’s transplant program, which has been at the forefront of advances in the field, Dr. Wee says.
Cleveland Clinic launched one of the world’s earliest kidney transplant programs in 1957. Pancreas and kidney-pancreas transplants began in the 1980s. The program has extensive experience with minimally invasive procedures, having performed its first laparoscopic donor nephrectomy in 1997, first laparoscopic single-port nephrectomy in 2007, and the world’s first single port robotically assisted extraperitoneal kidney transplant in 2019.
Advertisement
“We are very comfortable doing the most complex kidney transplants,” Dr. Wee says. “In 2024, the team performed 60 robotically assisted kidney transplants. This is the biggest volume for a single center not just in the United States but the world. This year, we expect to do more than 100. That is about a third of our total kidney transplants. So robotically assisted kidney-pancreas transplants were the logical next step.”
The patient had been diagnosed with type 1 diabetes at age 18. She struggled with management over the years and was hospitalized several times with diabetes-related ketoacidosis.
After referral to a nephrologist, she was diagnosed with end-stage renal disease and began peritoneal dialysis in 2021. Following discussions and evaluation with her Cleveland Clinic care team, she was placed on the transplant registry in 2024. A compatible deceased donor was identified and the transplant took place on Jan. 21, 2025.
In addition to Dr. Wee, the surgical team included lead robotic surgeon Mohamed Eltemamy, MD, Yi-Chia Lin, MD, and Venkatesh Krishnamurthi, MD.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a7de0338-f6bd-40cf-b247-207c8991fe97/kidney-pancreas-transplant)
The kidney and pancreas allografts are prepared at the backbench.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bb1e2233-227c-447d-b8c4-ea864ed75e42/kidney-pancreas-transplant)
Drs. Lin (left) and Eltemamy prepare the transplant recipient for implantation of the donor organs.
To prepare the patient, Drs. Eltemamy and Lin made a Pfannenstiel incision, dissected and retracted the rectus abdominus and entered the peritoneum. They placed a gel port sleeve to allow introduction of the donor organs into the abdomen, and four eight-millimeter ports at and above the umbilicus level to accommodate robotic instrumentation, then docked the robot. The left external iliac artery and vein were dissected, and peritoneal flaps were raised to accommodate the donor kidney.
Advertisement
Meanwhile, Drs. Wee and Krishnamurthi readied the kidney and pancreas allografts at the backbench.
The perinephric adipose tissue and adrenal gland were excised from the kidney to ensure homeostasis; branches from the renal vessels were ligated; the ureter was trimmed and spatulated; and a ureteral stent was placed. The kidney was placed in a glove to ease its eventual abdominal entry, then returned to a preservation bath.
The donor pancreas was prepared by performing a splenectomy. The donor duodenum was mobilized, shortened and oversewn. The mesentery root was oversewn. The portal vein was dissected. A Y-graft arterial reconstruction was completed by anastomosing the internal iliac artery to the splenic artery and the external iliac artery to the superior mesenteric artery. The pancreas was placed in a glove and returned to preservative.
The surgeons undertook the robot-assisted kidney transplantation first. The allograft was passed through the gel port sleeve and positioned in the patient’s right abdomen. Anastomoses of the donor renal vein to the external iliac vein and the renal artery to the external iliac artery were performed. Following clamp removal, excellent hemostasis and prompt perfusion of the kidney were observed. The ureteral stent was passed into the urinary bladder for drainage and anastomosed to the bladder mucosa.
Next, the donor pancreas was passed through the gel port sleeve into the left abdomen, lateral to the iliac vessels. Anastomoses of the donor portal vein to the external iliac vein, and the common iliac end of the donor iliac artery Y-graft to the external iliac artery, were performed. Unclamping confirmed hemostasis and appropriate vascularization of the pancreas. The allograft duodenum was hand-sewn to the recipient jejunum to enable enteric drainage of the pancreas.
After final inspection of the organs, the robot was undocked. The patient’s fascia and abdominal skin were sutured and her peritoneal dialysis catheter was removed.
The procedure lasted five hours.
The robotic-assisted surgery’s small incisions and minimal dissection area reduced the patient’s pain and analgesia needs. Opioids were discontinued on postoperative day two. She was discharged six days postoperatively, after resolution of her gastroparesis.
Now, “she has fully recovered,” Dr. Wee says.
The allografts are functioning normally. “Her sugar is well controlled, eliminating the need for insulin,” Dr. Eltemamy adds. “Simultaneously, she doesn’t need to undergo dialysis.”
With the success of the initial robot-assisted pancreas-kidney transplant, Dr. Wee and his colleagues are aiming to achieve the same expertise and productivity as Cleveland Clinic’s high-volume robot-assisted kidney transplant program.
“You have to be very proficient with using the robot,” he says. “We’ve been doing this a lot with kidney transplants. Now, we can easily go to the next step.”
Advertisement
Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more
Insights on bringing Cleveland Clinic even closer to becoming the best transplant enterprise in the world
Consensus statement aims to increase use of the perfusion technology and raise transplant volumes
AHA recommendations for pretransplant evaluation, peritransplant and long-term management
First-ever procedure restores patient’s health
The agent-based model aims to improve prediction accuracy
New guidelines expand on psychosocial, sexual health, cognitive and other issues
Consensus conference begins work on new recommendations for clinical care and research