Capecitabine-based approach shows promise in a population with few options
Low-dose capecitabine plus bevacizumab was well tolerated by patients with glioblastoma (GBM) and was associated with a reduction in circulating myeloid-derived suppressor cell (MDSC) levels and a rise in cytotoxic immune infiltration into the tumor microenvironment. So finds a Cleveland Clinic-led bench-to-bedside clinical investigation recently published in JCI Insight (2019;4[22]:e130748).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite aggressive treatment approaches, the median survival for patients with GBM is 14 to 18 months. The standard of care currently involves maximal safe surgical resection followed by concomitant radiation and chemotherapy with temozolomide, but this approach is often unsuccessful and leads to recurrent tumors and few options for patients.
“Similar challenges in other cancer types have been overcome with immune-modulating therapies, and this has sparked interest in modifying the immune system in glioblastoma,” says the study’s lead author, David Peereboom, MD, a medical oncologist in Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center. “While a number of immunomodulatory approaches are being evaluated, the immunosuppressive nature of the disease remains an obstacle.”
The study was prompted by mounting evidence, from Cleveland Clinic and elsewhere, that elevated levels of circulating MDSCs contribute to GBM. “Preclinical models suggested that low-dose chemotherapy reduces MDSCs,” notes corresponding author Justin Lathia, PhD, Co-Director of Cleveland Clinic’s Center of Excellence in Brain Tumor Research and Therapeutic Development, “but the use of this strategy in patients with glioblastoma required further study.”
To explore this approach, the researchers initiated a phase 0/I dose-escalation study to evaluate capecitabine’s ability to reduce circulating and tumoral MDSCs and to assess its tolerability alone and in combination with bevacizumab in patients with GBM. This work built on the team’s previous evaluation of this approach in a preclinical model (Stem Cells. 2016;34[8]:2026-2039).
Advertisement
The study involved 11 patients with recurrent GBM treated with low-dose capecitabine 5 to 7 days prior to surgery, followed by low-dose capecitabine and bevacizumab after surgery. Patients were enrolled in one of three escalating capecitabine dose cohorts, each given twice daily: 150 mg (n = 4), 300 mg (n = 3) or 450 mg (n = 4).
All three doses of capecitabine were reported to be well tolerated in combination with bevacizumab, with no serious adverse events related to the combination of the two drugs. Reported grade 3 adverse events were thromboembolism, dyspnea and anemia. Grade 1 and 2 events included fatigue (n = 4), hypertension (n = 3), nausea and vomiting (n = 2) and a small intracranial hemorrhage (n = 1).
Flow cytometry was used to evaluate peripheral blood MDSC concentrations before treatment, during surgical resection and after resection. Results showed that circulating MDSCs were higher after surgery relative to baseline in the 150-mg treatment group but were reduced from baseline in the 300- and 450-mg groups. In the 300- and 450-mg arms, increased cytotoxic immune infiltration was noted following capecitabine treatment compared with untreated GBM patients in a reference cohort.
These findings support the potential of low-dose capecitabine — given preoperatively, and then postoperatively with bevacizumab — for recurrent GBM, the researchers concluded. They noted that the therapy had an acceptable safety profile and that preliminary results indicated progression-free and overall survival rates comparable to those in historical controls.
Advertisement
Notably, tumor immune profiles were analyzed in this study using surgical samples gathered before bevacizumab treatment, excluding the possibility that bevacizumab contributed to the intratumoral effects observed. Additionally, although circulating MDSC levels were assessed while patients received combination chemotherapy, the MDSC changes were observed before bevacizumab administration began. “The decreasing MDSC levels also occurred in a capecitabine dose-dependent manner, making it unlikely that bevacizumab played a significant role,” the authors wrote.
“Based on comparisons of the immune populations among the capecitabine-treated groups, we determined that 300 mg twice daily is the optimal dose, leading to the most significant reduction in circulating MDSCs without impacting lymphoid populations required for an antitumor immune response,” says Dr. Lathia, who is also Vice Chair of the Department of Cardiovascular and Metabolic Sciences in Cleveland Clinic’s Lerner Research Institute.
“Additionally, through cytometry time-of-flight analyses, we observed that 5 to 7 days of priming the immune system with 300 or 450 mg of capecitabine twice daily enhanced the antitumor immune cell populations within the tumor, including CD8+ effector memory cells and NK cells,” he adds. He notes that while these results lack the statistical power to elucidate capecitabine’s complete effects on patients’ tumor immune responses, they support larger trials using the dose of 300 mg twice daily.
“Based on these findings, successful immunotherapy strategies for GBM will likely require an approach that involves targeting the immune suppressive effects of MDSCs as well as immune activation tactics to overcome GBM-induced immunosuppression,” Dr. Peereboom concludes.
Advertisement
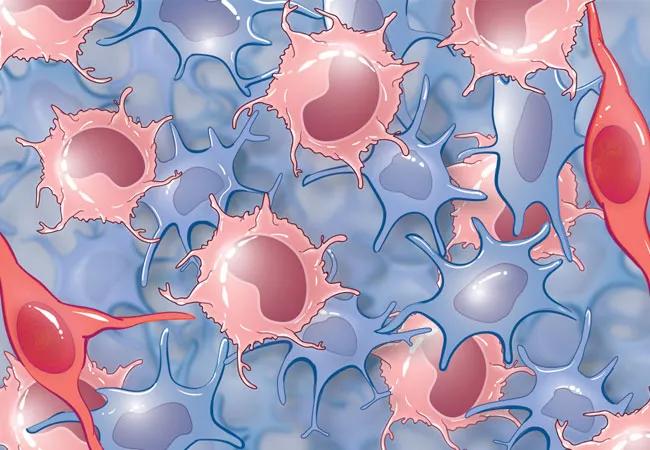
Illustration at top: Tumoral MDSCs (in pink) in the setting of glioblastoma.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology