Inhibitor stops DNA repair of cancer cells
The survival rate for patients with glioblastoma treated with the standard of care — radiation and chemotherapy — is poor. Most newly diagnosed patients with this aggressive brain cancer survive just 15 to 16 months.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
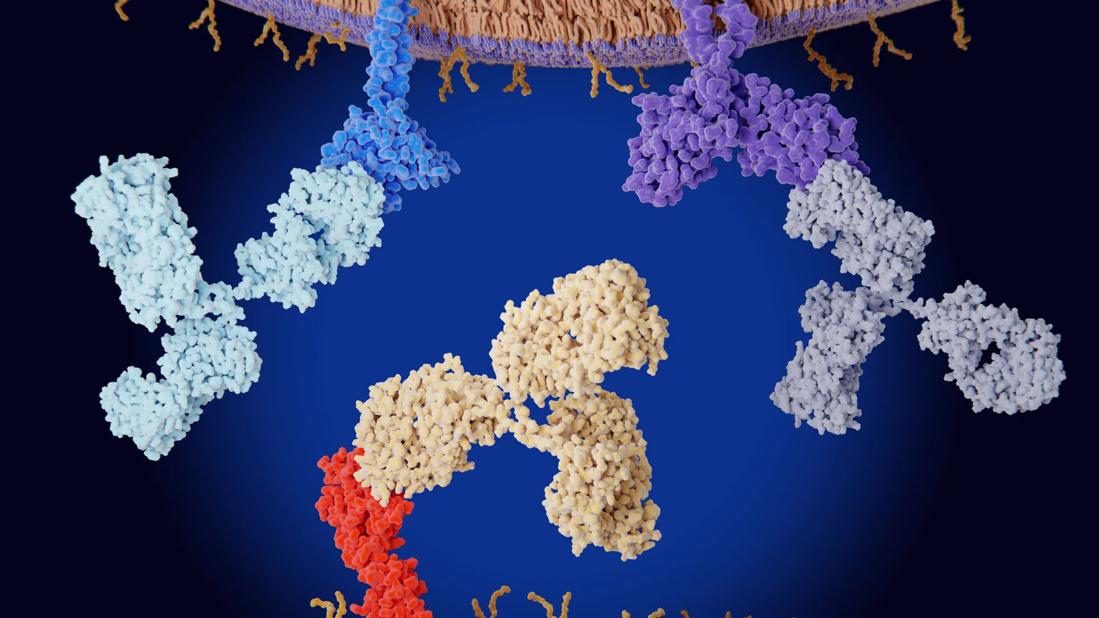
To improve those outcomes, researchers are combining the standard of care with checkpoint inhibitors involved in the cell cycle as an additional tool to kill cancer cells.
“Chemotherapy and radiation damage the DNA in cancer cells, but those cells can be repaired when they encounter checkpoints in the cell cycle,” says Manmeet Singh Ahluwalia, MD, FACP, the Dean and Diane Miller Family Endowed Chair in NeuroOncology at Cleveland Clinic. “Glioblastoma stem cells have been shown to be resistant to radiology, in part due to enhanced G2/M checkpoint activation and increased DNA repair.”
The G2/M checkpoint ensures that cells don’t begin mitosis before they have a chance to repair damaged DNA. If this checkpoint is inhibited, cells begin to divide before repairing their damaged DNA; this leads to the cell’s death.
Dr. Ahluwalia and colleagues from research institutions around the country recently launched a phase I dose-finding study combining radiation and chemotherapy with AZD1775, a small molecular inhibitor of a nuclear tyrosine kinase Wee1, a key regulator of the G2/M checkpoint.
The investigators chose AZD1775 because it can perform a dual-function as a DNA damage sensitizer (via Cdk1-mediated G2-checkpoint arrest) and as a cytotoxic agent (via Cdk2-mediated DNA-destabilization). A recent study reported at the 2016 American Society of Clinical Oncology (ASCO) annual meeting showed good penetration of the drug in a phase 0 trial of 20 patients(1).
The current study — which was accepted for presentation at ASCO 2017 in Chicago — is ongoing. So far Dr. Ahluwalia and colleagues have enrolled 51 patients and divided them into two groups: one group was given AZD1775 with concurrent radiation and chemotherapy, and one group was given AZD1775 with adjuvant chemotherapy.
Advertisement
For the concurrent group, maximum tolerable dose (MTD) was 200 mg. At 275 mg one patient had grade 3 fatigue and another had grade 4 thrombocytopenia and neutropenia. Two of the six total patients enrolled at 200 mg experienced dose-limiting toxicities (DLT): grade 4 neutropenia and grade 3 ALT elevation.
For the adjuvant group, the MTD was 425 mg. One of the six patients at this dose had DLT, a grade 4 decrease in absolute neutrophil count (ANC). At 500 mg, two of three patients experienced intolerable diarrhea despite prophylaxis.
For the combination cohort, IDD and PK/PD analysis is ongoing to inform the decision to proceed to phase 2 testing.
“The hope is that we can take this to a larger phase II study to look at the efficacy of this drug in patients with newly diagnosed glioblastoma,” Dr. Ahluwalia says. “Right now, we don’t have good therapeutic options for our patients.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient